
Blocked Tear Duct (Nasolacrimal Duct Obstruction)
A blocked tear duct occurs when your nasal passageways cannot properly drain tear liquid from your eyes. You may have itchy, irritated or watery eyes. Sometimes, babies are born with blocked tear ducts. A clogged tear duct may heal on its own, or you may need surgery. With treatment, most people experience total symptom relief.
What is a blocked tear duct?

The tears that moisturize your eye drain through a tiny opening in the corner of your eye. The liquid enters your nose, where your body absorbs and disposes of it.
A blocked tear duct is a full or partial obstruction (blockage) in the nasal (nose) passageways that drain tears. If you have a blocked tear duct, your eyes may be itchy, irritated and watery. Another name for a blocked tear duct is nasolacrimal duct obstruction. Lacrimal refers to tears.
How does the tear system work?
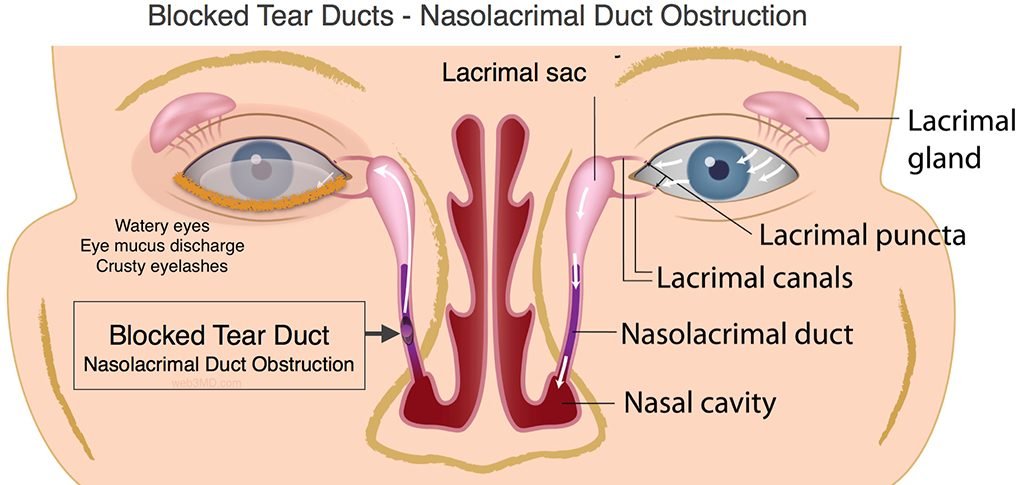
Typically, your tear system keeps your eyes slightly wet but not too watery. Your tear system has three parts:
Lacrimal glands : create tears.
Puncta : are small openings at your eye corner where tears flow out.
Nasolacrimal ducts : connect to the puncta and drain the rest of your tear fluid into the nose.
What are the tear ducts?
Tear ducts are another name for the nasolacrimal ducts. They form at the corner of your eye nearest your nose. They run underneath the skin and connect to your facial bones and nose.
How does a clogged tear duct affect my body?

When you have a clogged tear duct, tears can’t drain into the nose through the nasolacrimal ducts. Instead, your tears stay in your eye. The result is uncomfortable, watery eyes.
What is a partial tear duct blockage?
Sometimes, a narrow tear duct (dacryostenosis) can lead to a partial tear duct blockage. When you have a partial blockage, your tears may build up and not drain properly. This tear buildup can lead to infection. If you have a partial blockage, your provider will likely use similar treatments as a full blockage.
Who might get a blocked tear duct?
Blocked tear ducts are common in newborns. Usually, a blocked tear duct in a baby goes away without treatment.

Adults are more likely to develop a tear duct blockage if they have:
• Chronic eye inflammation, such as uveitis.
• Glaucoma.
• History of eye or sinus surgery.
• Previous cancer treatment, such as radiation therapy or chemotherapy.
CAUSES
Blocked tear ducts can happen to anyone of any age. Causes of blocked tear ducts include:
Age: As you get older, your puncta may naturally narrow.
Congenital blockages:
Some babies are born with tear ducts that are narrow or not fully formed (dacryostenosis).
Congenital obstruction of the lacrimal system is present in 1- 6% of newborn children.
Spontaneous resolution happens in 90-95% of cases during the first year of life. In the remaining 5-10% of children, 60% resolve spontaneously during the second year of life. After the fifth year, the probability of spontaneous resolution is minimal. The symptoms of the obstructed flow of tears are: tearing (epiphora), stickiness of the eyelashes due to mucopurulent discharge, and irritation of the periocular skin.
Infection : Chronic sinus infections or eye infections can lead to blockage.
Injury : Any eye injury near the tear ducts, even a scrape from tiny dirt particles, can cause a blockage.
Tumors : A tumor anywhere near the tear ducts, such as in the nose, can cause blocked tear ducts.
Symptoms of a blocked tear duct in adults?
Symptoms of a blocked tear duct in infants?
• Redness around the eye, usually from your baby rubbing the eye.
• Tears draining down the baby’s cheek instead of out of the eye corner.
• Tears pooling near the corner of the eye but not draining.
• Yellowish discharge or mucus in the baby’s eye.
What tests can help diagnose a blocked tear duct?
Tear drainage test:
Your provider places one drop of dye on each eye. If the dye does not drain from your eye, it could mean you have a blocked tear duct.
Eye imaging:
Your provider puts a special, safe dye in your eye. This dye travels through your tear drainage system. It shows up on an X-ray, CT scan or MRI to help your provider find the blockage.
Irrigation and probing:

Irrigation uses a fluid to clean out your tear ducts. Your provider may insert a small instrument through the corner of your eye to find the obstruction.
Treatment for a blocked tear duct in adults?
Probing:

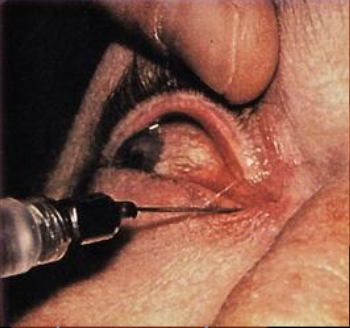

Probing is a procedure that is sometimes used to clear or open a blocked tear duct . The doctor inserts a surgical probe into the opening (punctum) of the tear duct to clear the blockage. Afterward, he or she may insert into the duct a tiny tube with water running through it. The water contains a fluorescein dye. If the doctor sees that dye has moved into the nasal cavity, he or she will know that probing worked. Often after probing, antibiotic eyedrops are used 4 times a day for 1 week.
Probing is rarely used as treatment for adults with a blocked tear duct. Probing is most often used when a baby:
• Is between 6 months and 13 months of age. Most blocked tear ducts open up on their own by 12 months of age.
• Has persistent tear duct infections and excessive tearing.
• Has a fully blocked duct. Partially blocked tear ducts often clear on their own by the time a child is 4 or 5 years old.
• Develops a bluish bulging area along the side of the nose (dacryocystocele).
• Becomes more and more irritable because of the blockage.
Medications:

If an eye infection caused the blockage, your provider may prescribe oral antibiotics or medicated eyedrops.
Stenting:
.jpg)
Your provider places a small, hollow tube (stent) through the puncta and into the tear duct. The tube allows tears to drain properly. The tubes stay in place for about three months. You will see a small portion of the tube out of the corner of your eye.
Balloon catheter dilation:

Your provider places a small, deflated balloon into the tear duct. Then your provider inflates the balloon a few times to clear the blockage. You are usually under general anesthesia (medication to help you remain asleep) for this procedure.
Snip punctoplasty:

Your provider makes two or three small incisions around your puncta. These incisions create a larger tear duct opening. Snip punctoplasty is a common treatment for partial blockages.
What is dacryocystorhinostomy for blocked tear ducts?
If less-invasive options don’t bring relief, your provider may recommend surgery. Providers usually use dacryocystorhinostomy (DCR). This procedure creates a new route to drain tears into your nose.
On the day of surgery, you receive anesthesia to help you stay calm and numb during the operation. During the procedure, your surgeon:

Treatment for a blocked tear duct in babies?

Often, a blocked tear duct in a newborn resolves without treatment. In the first few months of life, the baby’s tear ducts may mature and get rid of the blockage.
Sometimes, a baby still has a small piece of tissue blocking the flow of tears inside the nose. Your baby’s provider may teach you a special eyelid massage technique. This massage helps open the tissue so tears can drain as they should.
If a watch-and-wait approach does not work, providers may use dilation and flushing, balloon catheters or stents. These treatments work the same way in babies as they do in adults. However, providers use general anesthesia to keep babies still and calm during the procedure.
PREVENTION


Wash your hands frequently and thoroughly.
• Blurred vision.
• Crusting around the eyelids.
• Drainage, such as mucus or pus around the eyes.
• Redness in the white part of your eye.
• Swelling near your eye’s inner corner.
{{r.reply}}
Your comment was submitted for review. It will start display once it was approved by Admin
Comments