
What is glaucoma?

Glaucoma is a condition in which fluid pressure rises within the eye to an abnormally high level Without treatment, it can damage the optic nerve and lead to vision loss.
If it is diagnosed early, we may be able to prevent vision loss.
There is no cure for glaucoma, but treatment can slow or stop its progression.
This article will look at the causes, symptoms, and treatment of glaucoma. We will also explain the different types of glaucoma and possible surgical procedures.
What causes glaucoma?


The back of your eye continuously makes a clear fluid called aqueous humor. As this fluid is made, it fills the front part of your eye. Then, it leaves your eye through channels in your cornea and iris. If these channels are blocked or partially obstructed, the natural pressure in your eye, which is called the intraocular pressure (IOP), may increase. As your IOP increases, your optic nerve may become damaged. As damage to your nerve progresses, you may begin losing sight in your eye.
Who is at Risk of Glaucoma?



Types
There are several types of glaucoma, including:
• open-angle glaucoma
• closed-angle glaucoma
• low-tension glaucoma
• pigmentary glaucoma
• Congenital Glaucoma
• Secondary Glaucoma
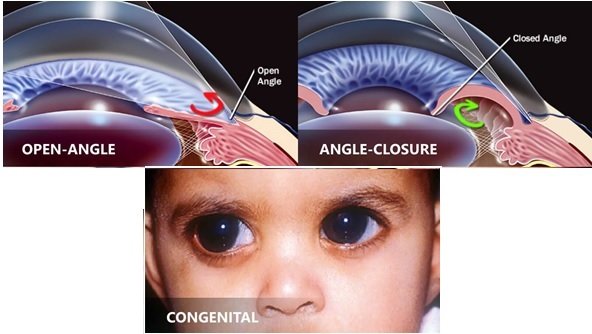
Open-angle glaucoma
Also known as chronic glaucoma, this is the most common type. It develops slowly, and a person may not notice any symptoms, even if slight vision loss occurs.
Many people with this type of glaucoma do not seek medical help until permanent damage has already occurred.
Closed-angle glaucoma
This is also known as acute angle-closure glaucoma. It can start suddenly with pain and rapid vision loss.
As the symptoms are noticeable, the individual will usually seek medical help, resulting in prompt treatment. This can prevent permanent damage.
Low-tension glaucoma
This is a rarer form of glaucoma in which eye pressure is not higher than the normal range but still causes damage that affects the optic nerve.
Experts know little about this condition, but it might be due to reduced blood supply to the optic nerve.
Congenital Glaucoma
Children born with congenital glaucoma have a defect in the angle of their eye, which slows or prevents normal fluid drainage. Congenital glaucoma usually presents with symptoms, such as cloudy eyes, excessive tearing, or sensitivity to light. Congenital glaucoma can run in families.
Secondary Glaucoma

Secondary glaucoma is often a side effect of injury or another eye condition, such as cataracts or eye tumors. Medicines, such as corticosteroids, may also cause this type of glaucoma. Rarely, eye surgery can cause secondary glaucoma.
Pigmentary glaucoma

This is a type of open-angle glaucoma that typically develops during early or middle adulthood.
It involves changes in the pigment cells that give color to the iris. In pigmentary glaucoma, the pigment cells disperse throughout the eye.
If the cells build up in the channels that drain fluid from the eye, they can upset the normal flow of fluids in the eye. This can lead to a rise in eye pressure.
How is Glaucoma diagnosed?

Ophthalmologists regularly check for glaucoma as part of a routine eye test. They can use several diagnostic tests:
Medical History
Your doctor will want to know what symptoms you’ve been experiencing and if you have any personal or family history of glaucoma. They’ll also ask for a general health assessment to determine if any other health conditions may be impacting your eye health, such as diabetes or high blood pressure.
Opthalmoscopy 
The eye doctor puts drops into the eye to widen the pupil, then examines the inside of the eye using a special light and magnifying glass.
Perimetry


The doctor carries out a visual field test to check the person’s peripheral (side) vision. The person looks straight ahead while the doctor presents a light spot in different places around the edge of their vision. This helps create a map of what the person can see.
Tonometry
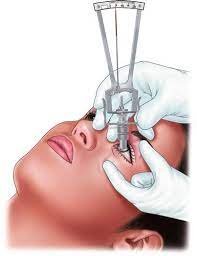

After using eye drops to numb the eye, the doctor measures the pressure in the eye with a device that either touches the cornea (applanation) or uses a puff of air.
Gonioscopy:
The doctor uses eye drops to numb the eyes, then places a type of contact lens on the eye. The lens has a mirror that that can show if the angle between the iris and the cornea is normal, too wide (open), or too narrow (closed).
Pachymetry
The doctor places a probe on the front of the eye to measure the thickness of the cornea. The doctor will take this into account when they assess all the results, as corneal thickness can affect eye pressure readings.
Treatment
Treatment aims to improve the flow of fluid from the eye, reduce fluid production, or both.
How is Glaucoma Treated?
Eye drops

Most people will use eye drops as initial treatment. These either reduce the amount of fluid the eye makes or improve drainage.
It is essential to follow a healthcare professional’s instructions carefully for the best results and to prevent adverse effects.
Examples of eye drops include:
• prostaglandins
• carbonic anhydrase inhibitors
• cholinergic agents
• beta blockers
• nitric oxide releasers
• rho kinase inhibitors
Adverse effects can include:
• stinging
• redness
• change in eye color or skin around the eye
• headaches
• dry mouth
• occasionally, retinal detachments or difficulty breathing
If the adverse effects persist, the doctor may change the dose or recommend a different option.
Surgery
If drugs do not help, or if the person cannot tolerate them, a doctor may recommend surgery.
Surgery usually aims to reduce the pressure inside the eye.


• Trabeculoplasty: The surgeon uses a laser beam to unblock clogged drainage canals, making it easier for fluid to drain out.
• Filtering surgery: If laser surgery does not help, the surgeon may open channels in the eye to improve fluid drainage.
• Drainage implant: This may help if glaucoma occurs in children or as a result of another health condition. The surgeon inserts a small silicone tube into the eye to improve drainage.
Treating acute angle-closure glaucoma:

Acute angle-closure glaucoma is a medical emergency.
A doctor will give pressure-reducing medications immediately.
They may use a laser procedure to create a tiny hole in the iris, allowing fluids to pass into the eye’s drainage system. This procedure is called an iridotomy.
Even if glaucoma only affects one eye, the doctor may treat both, because there is a risk that it might occur in the other eye, too.
Can Glaucoma Be Prevented?

There is no known way to prevent glaucoma, but early diagnosis and treatment can improve the chance of preventing vision loss.
It is essential to have regular eye checks because this is the only way to detect glaucoma in the early stages. We recommend having a baseline test at the age of 40. The doctor will use the results to detect future changes.
A doctor can advise an individual on how often they should have an eye test, depending on their risk level.
Can a person with Glaucoma go blind?
If your increased IOP can be stopped and the pressure returned to normal, vision loss can be slowed or even stopped. However, because there’s no cure for glaucoma, you’ll likely need treatment for the rest of your life to regulate your IOP. Unfortunately, vision lost as a result of glaucoma cannot be restored.
Is Glaucoma Hereditary?

Family history of open-angle and closed-angle. Glaucoma increases an individual’s risk of developing glaucoma.
Is open-angle glaucoma hereditary?
Open-angle glaucoma is hereditary; individuals with a family history of glaucoma are four to nine times more likely to develop glaucoma. If you have a family history of glaucoma, it is important to let your ophthalmologist know as soon as possible.
Is closed-angle glaucoma hereditary?
Closed-angle glaucoma is less common than open-angle glaucoma, and it typically occurs very suddenly. Though it is a less common type of glaucoma, it is still hereditary.
If you have a sibling or parent who has closed-angle glaucoma, your own risk for this type of glaucoma increases greatly. Keep your siblings informed if you are diagnosed with glaucoma, and ask them to do the same.
Glaucoma is hereditary, so be sure to know your family history and let your ophthalmologist know if glaucoma runs in your family. to schedule an exam and discuss any questions you have or the symptoms you are experiencing.
Childhood Glaucoma
Childhood glaucoma is a rare condition that may be inherited, caused by incorrect development of the eye’s drainage system before birth.

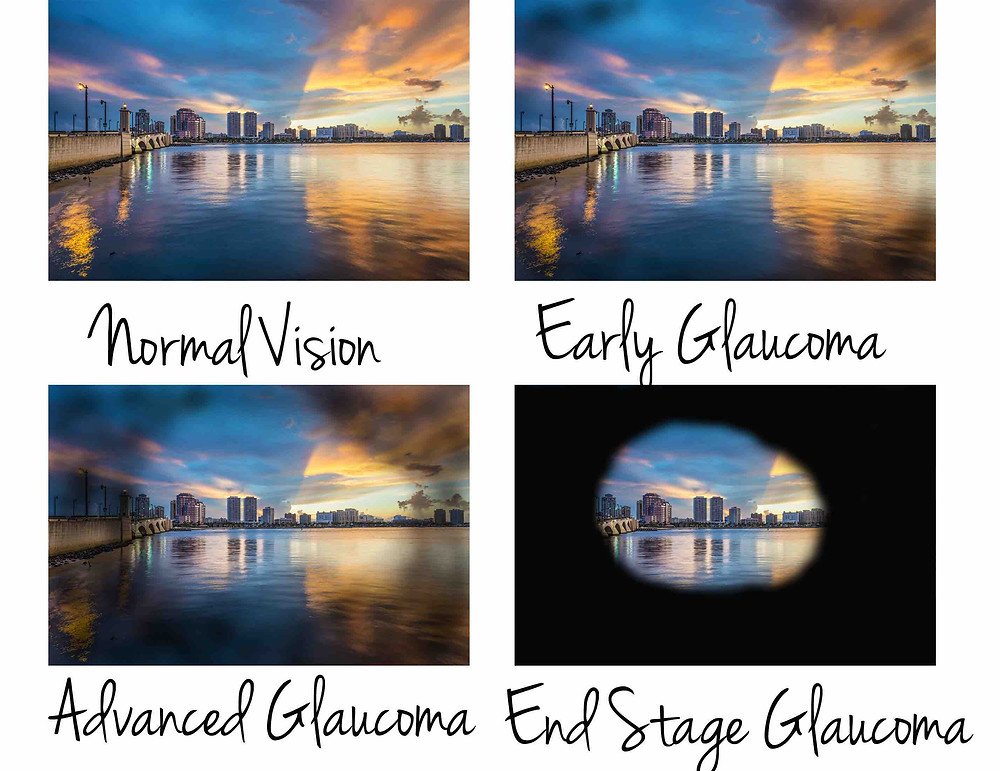
Normal vision Vision in glaucoma
Childhood glaucoma — also referred to as congenital glaucoma, pediatric, or infantile glaucoma — occurs in babies and young children. It is usually diagnosed within the first year of life.
This is a rare condition that may be inherited, caused by incorrect development of the eye’s drainage system before birth. This leads to increased intraocular pressure, which in turn damages the optic nerve.
How is it Treated?
In an uncomplicated case, surgery can often correct such structural defects. Both medication and surgery are required in some cases.
There are two main types of surgical treatments: filtering surgery and laser surgery. Filtering surgery (also known as micro surgery) involves the use of small surgical tools to create a drainage canal in the eye. In contrast, laser surgery uses a small but powerful beam of light to make a small opening in the eye tissue.
What to Expect
Thousands of children with glaucoma can live full lives. This is the ultimate goal of glaucoma management. Although lost vision cannot be restored, it is possible to optimize each child’s remaining vision. Equally important is to encourage your child’s independence and participation in his or her own self-care.
Symptoms
Signs and symptoms can include:

• light sensitivity (photophobia)
• corneal opacification (hazy gray cornea)
• enlarged eye and cornea
• epiphora (overflow of tears)
• vision loss
A cloudy cornea is the earliest and most common sign of childhood glaucoma. The healthy cornea is transparent. The loss of this transparency is caused by edema, or swelling of tissue from excess fluid. This occurs in the corneal epithelium (outermost layer of the cornea) and in the corneal stroma (middle layer of the corneal tissue). Careful inspection of the cornea may also reveal defects in its inner layer, which is further proof of a raised eye pressure (IOP).
In most cases of glaucoma affecting children under three years of age, the cornea and eye enlarges. Review of early photographs of your child may reveal the presence of glaucoma months before the diagnosis was actually made.
In addition to eye problems, secondary systemic (body) symptoms may occur. These secondary symptoms are especially common with acute glaucoma. Examples include irritability, loss of appetite, and vomiting. These symptoms may be misunderstood before the glaucoma is recognized. Young children with glaucoma are often unhappy, fussy, and poor eaters.
A slow chronic increase in eye pressure is probably not painful. In contrast, there is discomfort and pain when the eye pressure increases rapidly during an acute onset or with the rapid return of glaucoma following unsuccessful glaucoma surgery. Lowering high eye pressure relieves these painful symptoms quickly.
Summary
Glaucoma is a common eye condition that affects people as they get older. It happens when fluid does not drain from the eye, increasing pressure and the risk of damage to the optic nerve.
It may have no symptoms in the early stages but can lead to vision loss. Regular eye tests can help detect changes that will enable a person to start treatment, usually with eye drops. This treatment can slow or prevent vision loss.


{{r.reply}}
Your comment was submitted for review. It will start display once it was approved by Admin
Comments