4. Ophthalmic Migraine:
Ophthalmic (or ocular) migraine is a common term used to describe migraine characterized by symptoms including visual disturbances, blind spots, and blindness. These symptoms last about a minute before the migraine begins, and can occur with or without the head pain. Out of 200 people with migraine, one of them would have the experience of an ocular migraine.
5. Vestibular Migraine:
Vestibular migraine, often known as migrainous vertigo, refers to migraine accompanied by symptoms like vertigo, dizziness, and imbalance. People with vestibular migraine may feel the room spinning during the attack (external vertigo) as well as feel like they are moving when they are not (internal vertigo). The vertigo may worsen with certain motions such as standing up, looking down etc.
“[v]estibular migraine affects up to 3% of the adult population and affects up to 5 times more women than men”.
Diagnosing vestibular migraine is challenging in itself as there are other conditions that have similar vertigo symptoms, such as Benign Paroxysmal Positional Vertigo (BPPV), Ménière’s disease, and Transient Ischemic Attack (TIA) or “mini-stroke”.
6. Migraine with Brainstem Aura (Basilar Migraine):
Formerly known as basilar migraine, this type of migraine refers to migraine attacks with “aura symptoms originating from the base of the brain (brainstem) or both sides of the brain (cerebral hemispheres) at the same time.”
The symptoms of migraine with brainstem aura usually include two or more of the following: vertigo/dizziness, slurred speech, ringing in the ears, visual disturbances in both eyes, and loss of consciousness.
7. Abdominal Migraine:
Abdominal migraine, as the name suggests, is characterized by pain in the abdomen and occurs more frequently in young children, with symptoms lasting up to three days. These symptoms include nausea, vomiting, and dizziness. Children who experience migraine can often experience delayed development.
Migraine and Sound Sensitivity
Did you know that at least 35% Migraine patients have mentioned sound sensitivity as one of their migraine symptoms? When you experience sound sensitivity even the mere sound of a falling leaf could sound like a bomb explosion!?
Above are some of the sounds which annoys us the most during a migraine! Indeed, some sounds in our daily lives can become extremely unbearable to hear thanks to our heightened senses during an attack.
With migraine attacks, there is usually higher sensitivity to sensory stimuli which means that at least one of the senses of hearing, touch, sight, taste, and/or smell becomes more sensitive! Hearing and sight are most commonly affected in migraine attacks.
Phonophobia:
Phonophobia, or sound sensitivity, is one of the most common symptoms experienced by the migraine community. Phonophobia is simply discomfort from sound.
Consider it this way: everyone is usually uncomfortable with loud sounds. This is completely normal! But with phonophobia, the tolerance for sounds is significantly reduced. In other words, the discomfort levels associated with sounds are reached quicker.This means that sounds that generally may not discomfort people without phonophobia will be very discomforting for people with phonophobia. Some examples include the ones mentioned above like the sound of utensils clanking together, chewing noises, a clock ticking, etc.
This sensitivity to sound is typically noticed during a migraine headache and sometimes during the prodrome phase. Loud noises intensify the pain of the headaches, and the pain usually persists even when the noise is stopped.
Increased sensitivity to light also usually accompanies sensitivity to noise.
In an attempt to reduce the discomfort associated with sound sensitivity, many migraine patients often end up withdrawing into tranquil environments due to the notion that staying in a region with no noise will combat it. This may not always work for everyone – being in an extremely quiet environment can end up intensifying the headache pain since even the slightest sounds can cause significant discomfort.
It is important to note that some individuals may have low thresholds for sound by nature. These people may seem to be ‘better hearers.’ This is not usually the case with people experiencing migraine attacks, as migraine warriors simply have a higher discomfort to loud noises than people without migraine attacks due to the sensitive migraine brain.
The link between weather and migraine
Up to half of people living with migraine say that changes in the weather can trigger their attacks.
Not everyone responds to each weather change in the same way, either.Heat triggers migraine attacks in some people, while others get attacks when the temperature drops. Certain people are more sensitive than others to shifts in temperature and humidity.
In some cases, many different factors come together to trigger a migraine attack. For example, you might get an attack on humid days, but only if you’re also stressed or hungry.
Humidity changes:
In general, higher humidity and temperatures seem to set off migraine attacks. Sudden changes in humidity or temperature — up or down — might also be a factor.
Temperature changes:
3.jpg)
In the study, people who were sensitive to temperature got more migraine attacks during the winter. People who weren’t temperature- sensitive had more attacks in the summer, but to a lesser extent, no relationship between hot or cold.
Storms:
Lightning was linked to headaches in people living with migraine. However, it was unclear why this would be the case.Storms as a migraine trigger may be related to changes in air pressure.
Dry conditions:
Cold and dry air in the winter may result in dehydration and lead to migraine attacks.Higher humidity in warm weather is linked to a higher chance of migraine attacks.
Dusty environments:
The relationship between dust and migraine is likely tied to allergies. who tested positive for certain allergies, including dust, had more frequent migraine attacks. migraine may sometimes be associated with allergic rhinitis, a condition where your body reacts to certain allergens. Inflammation in response to allergens may be one cause of these migraine attacks.
Wind:
There’s little recent research on wind and migraine, though wind is often listed as a migraine trigger.
Barometric pressure:
Barometric pressure after drops before bad weather. Lower air pressure pushes less against the body, allowing tissues to expand. The answer has to do with blood vessels: When the pressure rises, blood vessels narrow, and when the pressure drops, blood vessels widen. There is increase in migraine attacks when the barometric pressure dropped even slightly.The authors say a drop in barometric pressure causes blood vessels in the brain to widen, which triggers the release of serotonin. As serotonin levels rise, they set off the visual phenomenon known as aura. When serotonin levels drop again, the blood vessels swell, which may trigger a migraine attack.
Symptoms
Migraines, which affect children and teenagers as well as adults, can progress through four stages: prodrome, aura, attack and post-drome. Not everyone who has migraines goes through all stages.
Prodrome:
One or two days before a migraine, you might notice subtle changes that warn of an upcoming migraine, including:
• Constipation
• Mood changes, from depression to euphoria
• Food cravings
• Neck stiffness
• Increased urination
• Fluid retention
• Frequent yawning
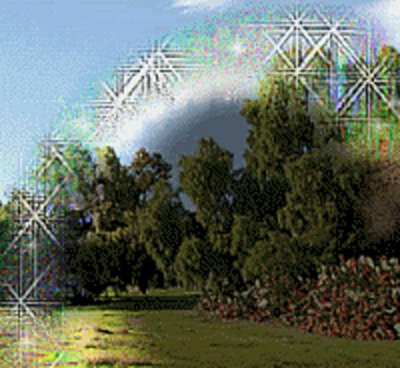
Aura: For some people, an aura might occur before or during migraines. Auras are reversible symptoms of the nervous system. They're usually visual but can also include other disturbances. Each symptom usually begins gradually, builds up over several minutes and can last up to 60 minutes.
Examples of migraine auras include:
• Visual phenomena, such as seeing various shapes, bright spots or flashes of light
• Vision loss
• Pins and needles sensations in an arm or leg
• Weakness or numbness in the face or one side of the body
• Difficulty speaking
Attack:
A migraine usually lasts from 4 to 72 hours if untreated. How often migraines occur varies from person to person. Migraines might occur rarely or strike several times a month.
During a migraine, you might have:
• Pain usually on one side of your head, but often on both sides
• Pain that throbs or pulses
• Sensitivity to light, sound, and sometimes smell and touch
• Nausea and vomiting
Post-drome:
After a migraine attack, you might feel drained, confused and washed out for up to a day. Some people report feeling elated. Sudden head movement might bring on the pain again briefly.
When to see a doctor
Migraines are often undiagnosed and untreated. If you regularly have signs and symptoms of migraine, keep a record of your attacks and how you treated them. Then make an appointment with your doctor to discuss your headaches.
Even if you have a history of headaches, see your doctor if the pattern changes or your headaches suddenly feel different.
See your doctor immediately or go to the emergency room if you have any of the following signs and symptoms, which could indicate a more serious medical problem:
• An abrupt, severe headache like a thunderclap
• Headache with fever, stiff neck, confusion, seizures, double vision, numbness or weakness in any part of the body, which could be a sign of a stroke
• Headache after a head injury.
• A chronic headache that is worse after coughing, exertion, straining or a sudden movement
• New headache pain after age 50
What triggers a migraine?
Migraine attacks can be triggered by a variety of factors. Common triggers include:
• Emotional stress. Emotional stress is one of the most common triggers of migraine headaches. During stressful events, certain chemicals in the brain are released to combat the situation (known as the "flight or fight" response). The release of these chemicals can bring on a migraine. Other emotions like anxiety, worry and excitement can increase muscle tension and dilate blood vessels. That can make your migraine more severe.
• Missing a meal. Delaying a meal might also trigger your migraine headache.
• Sensitivity to specific chemicals and preservatives in foods. Certain foods and beverages such as aged cheese, alcoholic beverages, chocolate and food additives such as nitrates (found in pepperoni, hot dogs and luncheon meats) and fermented or pickled foods may be responsible for triggering up to 30% of migraines.
• Caffeine. Having too much caffeine or withdrawal from caffeine can cause headaches when the caffeine level abruptly drops. Your blood vessels seem to become sensitized to caffeine and when you don't get it, a headache may occur. Caffeine is sometimes recommended by healthcare providers to help with treating acute migraine attacks but should not be used frequently.
• Daily use of pain-relieving medications. If you use medicine meant to relieve headache pain too often, that can cause a rebound headache.
• Hormonal changes in women. Migraines in women are more common around the time of their menstrual periods. The abrupt drop in estrogen that triggers menses can also trigger migraines. Hormonal changes can also be brought on by birth control pills and hormone replacement therapy. Migraines are generally worse between puberty and menopause since these estrogen fluctuations generally don’t occur in young girls and post-menopausal women. If your hormones are a strong factor in your migraines, you may have fewer headaches after menopause. Hormonal changes do not appear to trigger migraines in men.
• Light. Flashing lights, fluorescent lights, light from the TV or computer and sunlight can trigger you.
Other possible triggers include:
• Changing weather conditions such as storm fronts, barometric pressure changes, strong winds or changes in altitude.
• Being overly tired. Overexertion.
• Dieting, or not drinking enough water.
• Changes in your normal sleep pattern.
• Loud noises.
• Exposure to smoke, perfumes or other odors.
• Certain medications cause blood vessels to swell.
Migraines: Simple steps to head off the pain
Migraines cause pain as real as the pain of injuries — with one difference: Healthy habits and simple nonmedical remedies sometimes stop migraines before they start.
Medication is a proven way to both treat and prevent migraines. But medication is only part of the story. It's also important to take good care of yourself and understand how to cope with migraine pain when it strikes.
The same lifestyle choices that promote overall good health can also reduce the frequency and severity of your migraines.
Combining medication with behavioral measures and lifestyle can often be the most effective way to handle migraines.
Find a calm environment:
At the first sign of a migraine, take a break and step away from whatever you're doing if possible.
• Turn off the lights. Migraines often increase sensitivity to light and sound. Relax in a dark, quiet room. Sleep if you can.
• Try temperature therapy. Apply hot or cold compresses to your head or neck. Ice packs have a numbing effect, which may dull the sensation of pain. Hot packs and heating pads can relax tense muscles. Warm showers or baths may have a similar effect.
• Drink a caffeinated beverage. In small amounts, caffeine alone can relieve migraine pain in the early stages or enhance the pain-reducing effects of acetaminophen (Tylenol, others) and aspirin.
Be careful, however. Drinking too much caffeine too often can lead to withdrawal headaches later on. And having caffeine too late in the day may interfere with your sleep, which can also affect migraines.
• Medicines That Can Prevent Migraine Headaches:
It's the best situation: Stop a migraine before it starts. To do that, your doctor may consider these types of prescription drugs.
Anticonvulsants. These are medicines that prevent or reduce seizures. Your doctor may recommend topiramate valproic acid to prevent headaches. Anti-seizure drugs could make you sleepy. You may also find it harder to focus.
Beta-blockers. These relax your blood vessels. They’re often prescribed to control blood pressure. For migraines, your doctor may suggest atenolol, metoprolol, propranolol. Side effects include feeling depressed and having problems during sex.
Botulinum toxin (Botox). A doctor can inject small amounts around your face and scalp every 3 months to keep migraines from happening. This treatment is approved only for people who have headaches at least 15 days a month. The more often you have migraines, the better Botox seems to help.
Calcium-channel blockers. These include diltiazem and verapamil . They ease the narrowing of your blood vessels and are also given to treat heart disease. Side effects can include constipation and low blood pressure.
Antidepressants. Your doctor may prescribe tricyclic antidepressants like amitriptyline or nortriptyline. Some people gain weight and feel very tired when they take these. TCAs can also cause severe problems if you have heart disease or are pregnant. Research suggests that selective serotonin and norepinephrine reuptake inhibitors (SNRIs) such as duloxetine and venlafaxine may also help prevent migraines.
CGRP inhibitors. CGRP (calcitonin gene-related peptide) is a molecule involved in causing migraine pain. CGRP inhibitors are a new class of drugs that block the effects of CGRP. Atogepant, eptinezumab, erenumab, fremanezumab, and galcanezumab are approved to prevent migraine attacks. You give yourself a shot once a month with a pen-like device. Mild pain and redness at the injection site are the most common side effects. The long-term safety of CGRPs is unknown.
NSAIDs and triptans. If you're prone to migraines around your period, your doctor may have you take nonsteroidal anti-inflammatory drugs (NSAIDs), like naproxen or certain triptans, typically used to stop migraines once they've started, each month. You may be able to stave off an attack if you start a few days before your menstrual cycle starts and then stop a few days after your flow begins, for eg Sumatriptan, Naratriptan etc.
Natural Ways to Reduce Migraine Symptoms
Migraine attacks aren’t typical headaches. You may experience pounding pain, nausea, and sensitivity to light and sound. When a migraine attack or episode occurs, you’ll do almost anything to make it go away.
Natural remedies are drug-free methods of reducing migraine symptoms. These at-home treatments may help prevent the onset of migraine attacks or at least help reduce their severity and duration.
Keep reading as we take a look at 15 natural remedies that may help you manage migraine symptoms.
Note that migraine attacks may require treatment with prescription or over-the-counter (OTC) medication. Speak with a doctor about a treatment plan that works for you.
Eat wisely:
Your eating habits can influence your migraines. Consider the basics:
• Be consistent. Eat at about the same time every day.
• Don't skip meals. Fasting increases the risk of migraines.
• Keep a food journal. Keeping track of the foods you eat and when you experience migraines can help identify potential food triggers.
Avoid certain foods:
Diet plays a vital role in preventing migraine attacks. Many foods and beverages may be migraine triggers, such as:
• foods with nitrates, including hot dogs, deli meats, bacon, and sausage
• chocolate
• cheese that contains the naturally occurring compound tyramine, such as blue, feta, cheddar, Parmesan, and Swiss
• alcohol, especially red wine
• foods that contain monosodium glutamate (MSG), a flavor enhancer
• foods that are very cold, such as ice cream or iced drinks
• processed foods
• pickled foods
• beans
• dried fruits
• cultured dairy products, such as buttermilk, sour cream, and yogurt.A small amount of caffeine may ease migraine pain in some people. Caffeine is also in some migraine medications. But too much caffeine may cause a migraine attack. It may also lead to a severe caffeine withdrawal headache.
To figure out which foods and beverages trigger migraine attacks for you, keep a daily food journal. Record everything you eat and note how you feel afterward.
Sleep well
Migraines may keep you from falling asleep or wake you up at night. Likewise, migraines are often triggered by a poor night's sleep.
Here are some tips to encourage sound sleep.
• Establish regular sleep hours: Wake up and go to bed at the same time every day — even on weekends. If you nap during the day, keep it short. Naps longer than 20 to 30 minutes may interfere with nighttime sleep.
• Unwind at the end of the day: Anything that helps you relax can promote better sleep: listen to soothing music, soak in a warm bath or read a favorite book. But watch what you eat and drink before bedtime. Intense exercise, heavy meals, caffeine, nicotine and alcohol can interfere with sleep.
• Minimize distractions: Save your bedroom for sleep and intimacy. Don't watch television or take work materials to bed. Close your bedroom door. Use a fan to muffle distracting noises.
• Don't try so hard to sleep. The harder you try to sleep, the more awake you'll feel. If you can't fall asleep, read or do another quiet activity until you become drowsy.
• Check your medications. Medications that contain caffeine or other stimulants — including some medications to treat migraines — may interfere with sleep.
Eat wisely:
Your eating habits can influence your migraines. Consider the basics:
• Be consistent. Eat at about the same time every day.
• Don't skip meals. Fasting increases the risk of migraines.
• Keep a food journal. Keeping track of the foods you eat and when you experience migraines can help identify potential food triggers.
• Avoid foods that trigger migraines. If you suspect that a certain food — such as aged cheese, chocolate, caffeine or alcohol — is triggering your migraines, eliminate it from your diet to see what happens.
Exercise regularly:

During physical activity, your body releases certain chemicals that block pain signals to your brain. These chemicals also help alleviate anxiety and depression — and these two conditions can make migraines worse.
Obesity also increases the risk of chronic headaches. Maintaining a healthy weight through exercise and diet can provide additional benefits in managing migraines.
If your doctor agrees, choose any exercise you enjoy. Walking, swimming and cycling are often good choices. Just remember to ease into exercise gradually, as very vigorous exercise may trigger migraines.
Manage stress:
Stress and migraines often go hand in hand. You can't avoid daily stress, but you can keep it under control to help manage your migraines:
• Simplify your life. Don't look for ways to squeeze more activities or chores into the day. Instead, find a way to leave some things out.
• Manage your time wisely. Update your to-do list every day — both at work and at home. Delegate what you can, and divide large projects into manageable chunks.
• Take a break. If you feel overwhelmed, a few slow stretches or a quick walk may renew your energy for the task at hand.
• Adjust your attitude. Stay positive. If you find yourself thinking, "This can't be done," switch gears. Think instead, "This will be tough. But I can make it work."
• Enjoy yourself. Find time to do something you enjoy for at least 15 minutes every day. It could be playing a game, having coffee with a friend or pursuing a hobby. Doing something you enjoy is a natural way to combat stress.
• Relax. Deep breathing from your diaphragm can help you relax. Focus on inhaling and exhaling slowly and deeply for at least 10 minutes every day. It may also help to consciously relax your muscles, one group at a time. When you're done, sit quietly for a minute or two.
Keep a migraine diary:
2.jpg)
A diary may help you determine what triggers your migraines. Note when your migraines start, what you were doing at the time, how long they last and what, if anything, provides relief.
Until recently, avoiding migraine triggers was considered the best advice. But new research suggests this may actually increase sensitivity to potential triggers.
A more useful approach may be to gradually expose yourself to triggers, and learn to cope with these headache triggers by using behavioral management techniques. These may include identifying and challenging negative thoughts, relaxation training, and stress reduction. More research is needed to understand if and how this approach is more effective in managing migraines.
Strive for balance:

Living with migraines is a daily challenge. But making healthy lifestyle choices can help. Ask your friends and loved ones for support.
If you're feeling anxious or depressed, consider joining a support group or seeking counseling. Believe in your ability to take control of the pain.
Natural Ways to Reduce Migraine Symptoms
Migraine attacks aren’t typical headaches. You may experience pounding pain, nausea, and sensitivity to light and sound. When a migraine attack or episode occurs, you’ll do almost anything to make it go away.
Natural remedies are drug-free methods of reducing migraine symptoms. These at-home treatments may help prevent the onset of migraine attacks or at least help reduce their severity and duration.
Keep reading as we take a look at 15 natural remedies that may help you manage migraine symptoms.
Note that migraine attacks may require treatment with prescription or over-the-counter (OTC) medication. Speak with a doctor about a treatment plan that works for you.
1. Avoid certain foods:

Diet plays a vital role in preventing migraine attacks. Many foods and beverages may be migraine triggers, such as:
• foods with nitrates, including hot dogs, deli meats, bacon, and sausage
• chocolate
• cheese that contains the naturally occurring compound tyramine, such as blue, feta, cheddar, Parmesan, and Swiss
• alcohol, especially red wine
• foods that contain monosodium glutamate (MSG), a flavor enhancer
• foods that are very cold, such as ice cream or iced drinks
• processed foods
• pickled foods
• beans
• dried fruits
• cultured dairy products, such as buttermilk, sour cream, and yogurt
A small amount of caffeine may ease migraine pain in some people. Caffeine is also in some migraine medications. But too much caffeine may cause a migraine attack. It may also lead to a severe caffeine withdrawal headache.
To figure out which foods and beverages trigger migraine attacks for you, keep a daily food journal. Record everything you eat and note how you feel afterward.
2. Apply lavender oil:

Inhaling lavender essential oil may ease migraine pain. Lavender oil may be inhaled directly or diluted with a carrier oil and applied in small amounts to your temples.
A 2016 randomized controlled study found evidence that 3 months of lavender therapy as a prophylactic therapy, meaning taken before a migraine attack begins, reduced frequency and severity of migraine attacks. However, research is still limited.
A 2020 review of studiesTrusted Source published in the journal Phytotherapy Research examined the ability of various herbal treatments, including lavender therapy for migraine. The authors found mixed or limited evidence to support the use of butterbur and feverfew for treating migraine but didn’t note that current research supports the use of lavender.
According to the authors, many studies had a high risk for bias, and more high quality research is needed.
3. Ginger:
2.jpg)
Ginger is known to ease nausea caused by many conditions, including migraine. It may have pain-relieving benefits for migraine attacks. According to a 2020 review of studiesTrusted Source, one randomized controlled study found evidence that ginger may have beneficial activity.
More research is needed to understand the extent and usefulness of ginger for treating migraine-related pain.
Add magnesium to your diet:
Magnesium deficiency is linked to headaches and migraine. Magnesium oxide supplementation may help prevent migraine with aura. It may also prevent menstrual migraine (hormone headaches).
A 2021 studyTrusted Source found that 500 milligrams of magnesium oxide taken twice a day for 8 weeks was as effective as the medication valproate sodium for preventing migraine without significant side effects.
You can get magnesium from foods that include:



• almonds
• sesame seeds
• sunflower seeds
• Brazil nuts
• cashews
• peanut butter
• oatmeal
• eggs
• milk
.jpg)







1.jpg)
.jpg)

3.jpg)








2.jpg)








2.jpg)



2.jpg)



Comments