.jpg)
SUPERFICIAL PUNCTATE KERATITIS (MADRAS EYE)
DR. SURESH EYE HOSPITAL
THENGAPATTANAM ROAD, VETTUMANI, MARTHANDAM
PH. NO: 7200204030

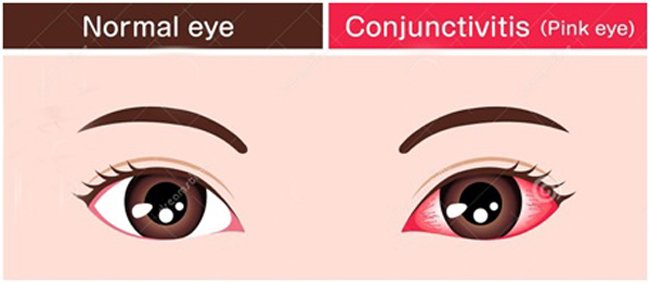
This disease is caused by a virus called adenovirus. This disease is also known by many names as Chennai Eye, Red Eye, Madras Eye, etc Let's call this Superficial Punctate Keratitis in English. Madras Eye is a common name for Conjunctivitis caused by the bacteria, chlamydia, virus and allergies.
It was Dr. Grid Patrick who introduced the disease to the world. It is also known as Chennai Eye Disease as it was discovered by the Dr. Patrick working at the second oldest Eye Hospital in the world ie Egmore Eye Hospital.


The virus spreads more during hot weather. The disease is rare in cold mountains. For 10 years I worked as an ophthalmologist in Munnar area and never saw a single Madras Eye patient.
Keratitis is an inflammatory condition that affects the cornea of your eye. The cornea is the clear part that covers both the iris and the pupil. Keratitis can be caused by an infection or injury to the eye.
Superficial Punctate Keratitis: Causes:
There are many different causes of superficial punctate keratitis. Most involve damage or irritation to the cornea of the eye. For example, when:

All these causes can damage the cells of the cornea and lead to superficial punctate keratitis.
Overexposure of the eyes to sunlight is one cause of superficial punctate keratitis.
How it spreads: The virus infected person spreads from the area he touches and the objects he uses. The general spread of the disease occurs when we touch people with the disease or the products they use towels, computers, etc. The disease does not spread because we see their eyes.

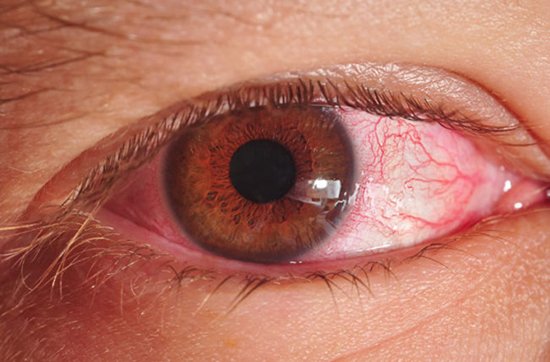
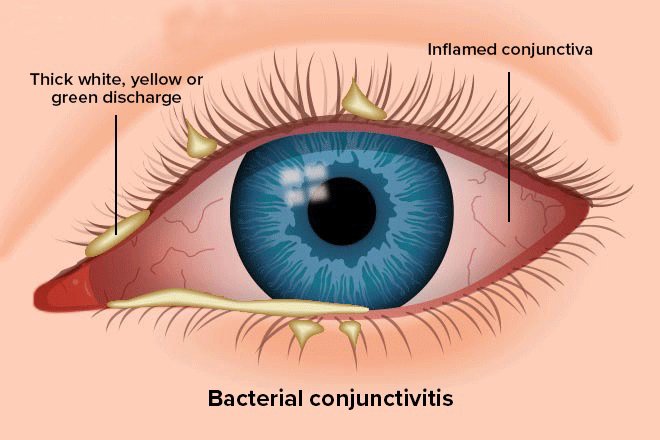
• Symptoms of the disease: Reddish discoloration of the white part of the eye, Light yellow or white discharge, Light Sensitivity, swelling of the eyelid. In the morning there may be sores or polyps in the form of small dots on the eyelid that close the white of the eye.



If the eyelids are stuck unable to open when you wake up, small sores on the iris can cause blurred vision and good irritation. There may be pain or a small lump with pain in the front of the ear.
Infectious causes of Keratitis:
Infectious keratitis is caused by one of the following:
Viruses: Viral keratitis is primarily caused by the herpes simplex virus, which progresses from conjunctivitis to keratitis.

Bacteria: Pseudomonas aeruginosa and Staphylococcus aureus are the two most common types of bacteria that cause bacterial keratitis.It mostly develops in people who use contacts improperly.
Fungi: Fungal keratitis is caused by Aspergillus, Candida, or Fusarium. As with bacterial keratitis, fungal keratitis is most likely to affect those who wear contact lenses. However, it’s also possible to be exposed to these fungi outdoors
Parasites: An organism called Acanthamoeba has become more common in the United States in those wear contact lenses. The parasite lives outdoors and may be picked up by swimming in a lake, walking in a wooded area, or getting infected water on your contact lenses. This type of infection is called Acanthamoeba keratitis.
Noninfectious causes of keratitis:
Possible noninfectious causes of keratitis include:


Diagnosis:
Diagnosing keratitis typically involves the following:
• Eye exam.


Although it may be uncomfortable to open your eyes for the exam, it's important to have your eye care provider examine your eyes.
• Penlight exam.

Your eye doctor may examine your eye using a penlight, to check your pupil's reaction, size and other factors. A stain may be applied to the surface of your eye. Used with the light, this stain makes it easier to see damage to the surface of the cornea.
• Slit-lamp exam.

Your eye care provider will examine your eyes with a special instrument called a slit lamp. It provides a bright source of light and magnification to detect the character and extent of keratitis, as well as the effect it may have on other structures of the eye. Viral eye disease requires mandatory testing. The examination may include visual impairment corneal damage and assessment of the internal systems of the eye. Consult a doctor to prevent scars and loss of vision. This include slit lamp Examination, Lymph node check and Fluorescein eye stain.
blood test:
Apart from complete blood test, Rapid Adenovirus screening / PCR Test can be done to diagnose and confirm adenovirus infection.
• Laboratory analysis.

Your eye care provider may take a sample of tears or some cells from your cornea for laboratory analysis to determine the cause of keratitis and to help develop a treatment plan for you.
Treatment:
Noninfectious keratitis:
Treatment of noninfectious keratitis varies depending on the severity. For example, with mild discomfort from a corneal scratch, artificial tear drops may be the only treatment. However, if keratitis is causing significant tearing and pain, topical eye medications may be necessary.
Infectious keratitis:
Treatment of infectious keratitis varies, depending on the cause of the infection.
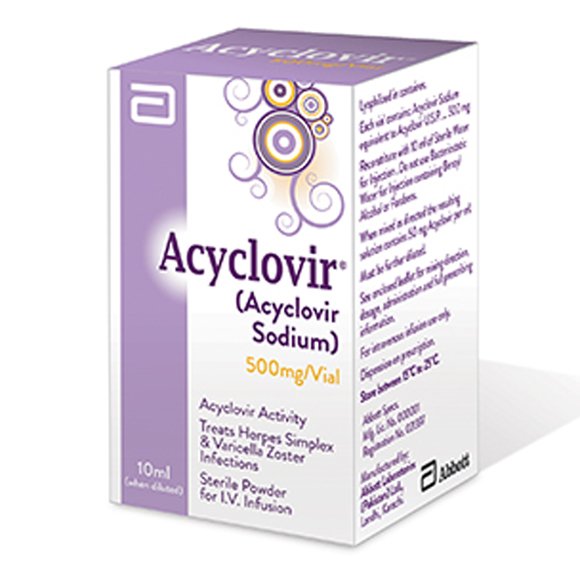
• Viral keratitis: If a virus is causing the infection, antiviral eye drops and oral antiviral medications may be effective. Other viruses need only supportive care such as artificial tear drops.

• Bacterial keratitis: Antibiotic eye drops are the primary treatment for bacterial keratitis. Depending on the severity of the infection, drop frequency can range from around four times a day to every 30 minutes, even during the night. Sometimes oral antibiotics are used as a supplement.
• Fungal keratitis: Keratitis caused by fungi typically requires antifungal eye drops and oral antifungal medication.
• Acanthamoeba keratitis. Keratitis caused by the parasite acanthamoeba can be difficult to treat. Antiparasitic eye drops are used, but some acanthamoeba infections are resistant to medication and can require treatment for several months. Severe cases of acanthamoeba keratitis may require a cornea transplant.
If keratitis doesn't respond to medication, or if it causes permanent damage to the cornea that significantly impairs your vision, your eye care provider may recommend a cornea transplant.
How long does it take to completely heal: This may take two to four weeks.
Medical treatment: If you put warm compresses on the eyes, the blood flow to the eyes will increase and the disease will decrease quickly. Take a cotton swab and soak it in water to remove discharge or. Drink 2 litres of water daily, eat at the right time and good sleep will help you to recover fast.

Use prescription drugs:


You can take head bath, it is better to see a doctor once the vision is clear. (Sight may be affected if the sore becomes scarred) May go away when the eyes become red.
Prevent the spread of disease:


Self-Hygiene Requirement Patient Shirts Other Fabrics, Bed Sheet, Handkerchief, Pillow Text, Towel should be changed daily. Avoid rubbing the eyes with your hands. Wear sunglasses to avoid exposure to sunlight. It is necessary to wash the hands after putting the medicine in the eye or touching the eyes. Start treatment and limit contact with others until symptoms begin to improve. We can avoid using the products that the victims use like bed sheets, towels, computer things, etc. clean the places the patient touched with disinfectant. It is better to use glasses both for patients and others nearby.
Virus: This disease can spread from the injected persons from 4 to 7 days after infection in adenovirus type 8 and 19.
1.jpg)
.jpg)
{{r.reply}}
Your comment was submitted for review. It will start display once it was approved by Admin
Comments