1.jpg)
CONJUNCTIVITIS / RED EYE /MADRAS EYE

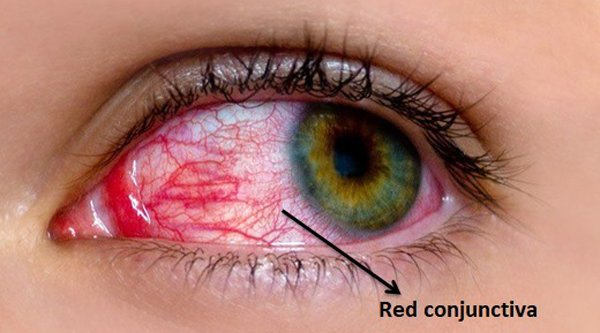
Conjunctivitis or Red eye, is inflammation of the membranes (conjunctiva) covering the white parts of the eyes and the membranes on the inner part of the eyelids.
Common Symptoms and Signs:
Red eye is characterized by reddening of the conjunctiva of the eyes, discharge from the eyes, and can be accompanied by other signs of infection like sinus congestion and runny nose.
Common Red eye symptoms and Signs



• Cough
• Earache
• Eye Discharge
• Eye Pain
• Eye Redness
• Itching Eyes
• Pus Drainage From Eye
• Runny Nose
• Sinus Congestion
• Swollen Eyelids
• Swollen Lymph Nodes
• Tearing
Causes of conjunctivitis (Red eye):
Allergic, viral, and bacterial are the three main types of red eye:
1. Viral conjunctivitis (Red eye):

Viruses responsible for red eye include:
• adenovirus — by far the most common.
• herpes virus — uncommon but more dangerous.

The leading cause of a red, inflamed eye is a viral infection. Adenoviruses are the type of virus that is most commonly responsible for the infection. Other viruses that can cause red eye include
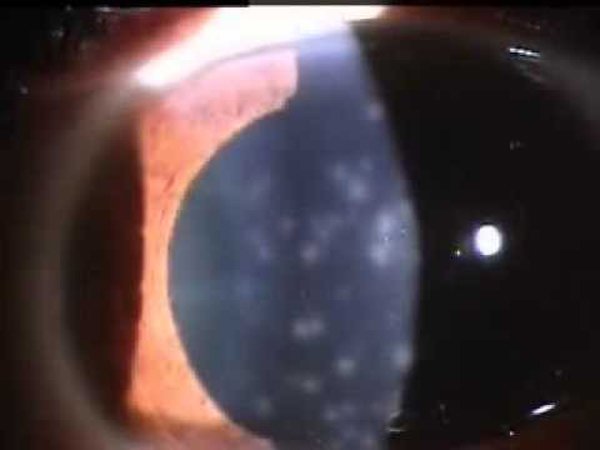
To know more details about EPIDEMIC KERATOCONJUNCTIVITIS please click here: SUPERFICIAL PUNCTATE KERATITIS (MADRAS EYE)
2. Bacterial conjunctivitis (Red eye):

IN INDIA VIRAL AND BACTERIAL CONJUNCTIVITIS ARE CALLED MADRAS EYE.
3. Chlamydia conjunctivitis (Red eye):
Red eye due to infection with chlamydia is an uncommon form of bacterial red eye.
• Chlamydia redeye symptoms are similar to bacterial redeye symptoms.

• Chlamydia can cause redeye in adults and babies. It is a cause of red eye in adolescents and adults that can be sexually transmitted.
How can you tell if red eye is bacterial or viral?
Although the symptoms of red eye can be the same regardless of cause, your healthcare provider uses a few signs to help determine if red eye is bacterial or viral:
Age: Viruses cause most cases of red eye in adults. Bacteria and viruses each cause about the same number of red eye infections in children.

Ear infection: If your child has bacterial conjunctivitis, it’s common for them to also have an ear infection at the same time.
Amount of discharge: A lot of discharge from your eye is usually a sign of a bacterial infection.

Color or tint of the whites of eye: Salmon (light pink) color may be a sign of a viral infection. A reddish color is more likely to be a bacterial conjunctivitis.

If it’s in one or both eyes: If you have red eye that’s in both eyes, a virus is probably causing it.
Diagnosis and Tests:
How is red eye diagnosed?
1. Medical History:
Your ophthalmologist can rule out many causes of conjunctivitis simply by asking about your symptoms and how they came about. He or she also asks whether you’ve been in close contact with other people who have conjunctivitis and if any irritant has come into contact with your eye.
2. Torch light (flash light):

A torch light is an instrument used by an ophthalmologist to examine the eye of a patient. A good torch light should give a circular patch of light of nearly uniform brightness
.
3. Visual Acuity Tests:

Doctors also check to see if conjunctivitis has affected your vision by conducting a visual acuity test. This test checks to see how well you can read letters or symbols from 20 feet away, while covering one eye at a time.
4. slit lamp exam:
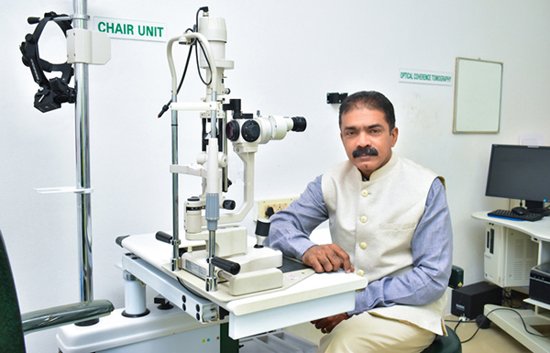
Most of the time, your doctor can diagnose conjunctivitis by using a slit lamp—an instrument that consists of a microscope and a high-energy beam of light. During a slit-lamp exam, your ophthalmologist shines a thin beam of light into your eye. This beam allows your doctor to examine the entire eye, including the conjunctiva; the sclera, or the white of the eye; the iris; and the cornea.
For a more detailed look at the eye, your doctor may put a drop of a yellow dye called fluorescein into your eye, which allows him or her to see any damage to the surface of the eye.
5. Lab test:

For culture to isolate the organism. If you have had conjunctivitis for more than two or three weeks and it has not gone away on its own or with the help of home treatments, your doctor may want to perform an eye culture. During this test, your doctor takes a sample of the cells on the inside of your eyelids with a cotton swab and sends it to a laboratory to be examined by a pathologist.
A pathologist, who studies diseases under a microscope, can determine whether your conjunctivitis is caused by viruses or bacteria. This helps your doctor determine the most effective treatment.
SPREAD:
How did I catch conjunctivitis?
You can catch viral and bacterial conjunctivitis from direct contact with eye discharge from a person with conjunctivitis. You can also catch it from contact with objects that were contaminated with infectious eye secretions, such as towels, face washers and tissues.
How can you prevent conjunctivitis?
Practicing good hygiene is one of the best ways to avoid and stop the transmission of conjunctivitis:



What you should do if you are living closely with a Conjunctivitis patient should take necessary precautions to prevent this virus from spreading. Here are a few preventive tips for the same:

• Maintain a high level of hygiene at home especially if one or more members of the family are suffering from conjunctivitis. Wash your bed sheets, pillowcases & towels in hot water and detergent to prevent spreading the infection. Use a good quality disinfectant to keep your home clean & free from germs.
.jpg)
• Do not share personal belongings
• Always wash your hands thoroughly between regular intervals and avoid touching your face & eyes too often.


• Consume more of immune boosting foods. Green leafy vegetables and orange colored fruits contain beta carotene which helps in improving the immune system thereby minimizing the chances of contracting this eye infection.

• Opt for disposable tissues instead of handkerchiefs or towels to dab eyes. After use, do not throw these tissues on the floor or any area where they could be easily accessible to others.

• Avoid visiting crowded places. When outdoors, always cover up your eyes with sunglasses. Doing so will prevent the eyes from coming in contact with dust & foreign particles, which could trigger conjunctivitis at a later stage
• Avoid wearing & sharing eye make-up and/or contact lenses
TREATMENT:
How to Prevent Madras eye from Spreading?



Treatment - Viral Conjunctivitis(Red eye):

If your conjunctivitis is caused by a viral infection, there are no specific treatments. Your body fights the virus on its own.
Treatment - Bacterial Conjunctivitis(Red eye):
• First, if the cause is a bacterial infection, an antibiotic will be needed to help the infection-fighting immune system to kill this infection.


• Types of topical ophthalmic (eye drops) antibiotics often used for redeye include besifloxacin (Besivance), gatifloxacin (Zymaxid), levofloxacin (Levaquin, Quixin, Iquix), moxifloxacin (Moxeza, Vigamox), tobramycin.
• Secondly, if someone is experiencing other symptoms such as a runny nose, cough, earache, etc., there is a good chance that these symptoms are caused by the same bacteria, and an oral antibiotic may also be needed to treat this infection along with the antibiotic eye drops or ointment for the eyes.
Treatment - Chlamydia Conjunctivitis (Red eye):


Chlamydia redeye is typically treated with erythromycin or oral tetracycline (Sumycin), except in children less than 8 years of age, because of possible discoloration of the teeth.
OUTLOOK/ PROGNOSIS:
How long does red eye last?

If you have bacterial conjunctivitis, it should improve within a week. Take any medicine as instructed by your healthcare provider, even if your symptoms go away.
Viral conjunctivitis usually lasts from four to seven days. It can take up to 14 days to fully resolve.
When can I return to daycare, school or work if I have red eye?
You or your child can usually go back to daycare, school or work as soon as your symptoms go away. This might be as soon as 24 hours after antibiotic treatment for a bacterial infection and between two and seven days after viral infection.
Your eyes shouldn’t have any:
• Yellowish discharge.
• Crusting on your eyelashes or in the corners of your eyes.
• Pink color.
Be sure to check with your healthcare provider about when it’s safe to return. If an allergy or something else that’s not contagious caused your red eye, you don’t need to stay home.
Should I go to the doctor for red eye?
You don’t necessarily need to see a doctor for red eye. Most of the time, you can treat the symptoms at home until it goes away on its own. But you should never hesitate to call your healthcare provider if you have any concerns.
Some symptoms can be a sign of a serious problem, such as an ulcer, which can result in permanent vision loss. Call your healthcare provider or seek medical care right away if you experience:



• An increase in sensitivity to light, especially if it’s severe.
• Blurred vision or decrease in vision.
• Eye pain.
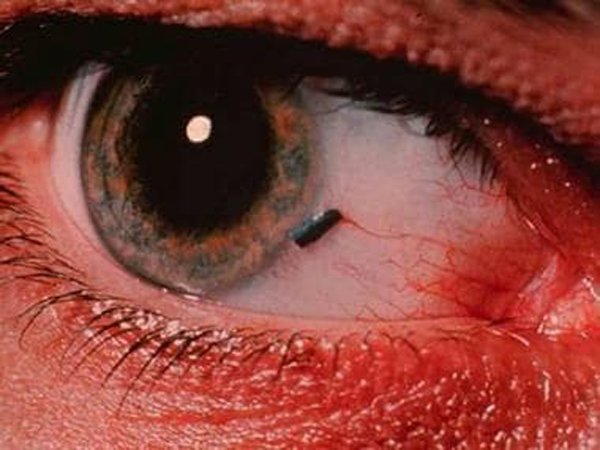
• Feeling like there is something stuck in your eye.
• Large amount of discharge from your eyes.
• Worsening symptoms.
QUICK HOME REMEDIES FOR RED EYE:
Bacterial and viral redeye home remedies:
If one or both of your eyes are red and uncomfortable, it could be allergic red eye, viral red eye or bacterial red eye. Sometimes it's easy to figure out what kind of red eye you have and other times only a doctor can tell what's causing the problem.
• Viral redeye is like a common cold in the eye. There is no treatment for the virus and usually you just have to let it heal on its own. Viral red eye should go away within a week or two without treatment.
• Bacterial redeye usually produces more mucus or pus than viral or allergic red eye. Bacterial red eye can be treated with antibiotics prescribed by a doctor.
To reduce the symptoms of bacterial or viral red eye you can:
• Take ibuprofen or another over-the-counter pain killer.
• Use over-the-counter lubricating eye drops (artificial tears).
• Put a warm, damp washcloth over your eyes for a few minutes. To make this warm compress:
.jpg)
• Soak a clean washcloth in warm water then wring it out so it’s not dripping.
.jpg)

If your eyelids are sticking together, a warm washcloth can loosen the dried mucus so you can open your eyes.
NON CONTAGIOUS FORMS OF RED EYE:
1. Chemical conjunctivitis (Red eye):
Chemical redeye can result when any irritating substance enters the eyes. Common offending irritants are


• household cleaners,
• sprays of any kind,
• smoke,
• a foreign body in the eye,
• smog,
• industrial pollutants.
Prompt, thorough washing of the eyes with very large amounts of water is very important if an irritating substance enters the eye. A doctor or local poison control center should be contacted at once, even if the irritant or chemical is thought to be safe, as some of the most common household products like bleach and furniture polish can be very damaging.
2. Allergic conjunctivitis(Red eye):


To know more details about Allergic conjunctivitis please click here: ALLERGIC CONJUNCTIVITIS
.jpg)
2.jpg)
{{r.reply}}
Your comment was submitted for review. It will start display once it was approved by Admin
Comments