
Overview

(PLEASE CLICK HERE FOR IMAGE FORMAT: DIABETIC RETINOPATHY)
(PLEASE CLICK HERE FOR TAMIL IMAGE FORMAT: DIABETIC RETINOPATHY)
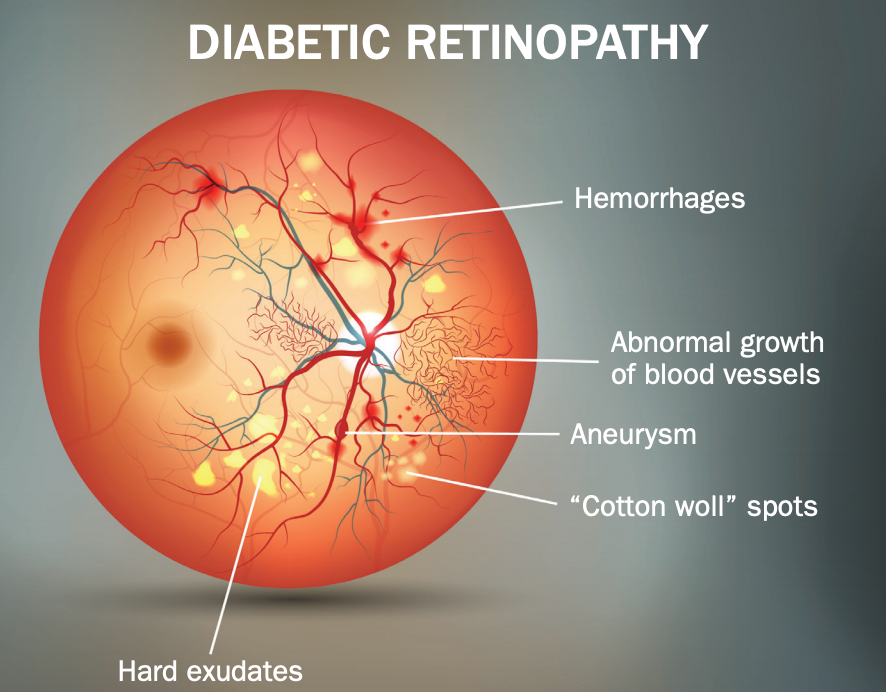
Diabetic retinopathy is a diabetes complication that affects your eyes. It's caused by damage to the blood vessels of the light-sensitive tissue at the back of the eye (retina).
At first, diabetic retinopathy might cause no symptoms or only mild vision problems. But it can lead to blindness.
The condition can develop in anyone who has type 1 or type 2 diabetes. The longer you have diabetes and the less controlled your blood sugar is, the more likely you are to develop this eye complication.
Symptoms:

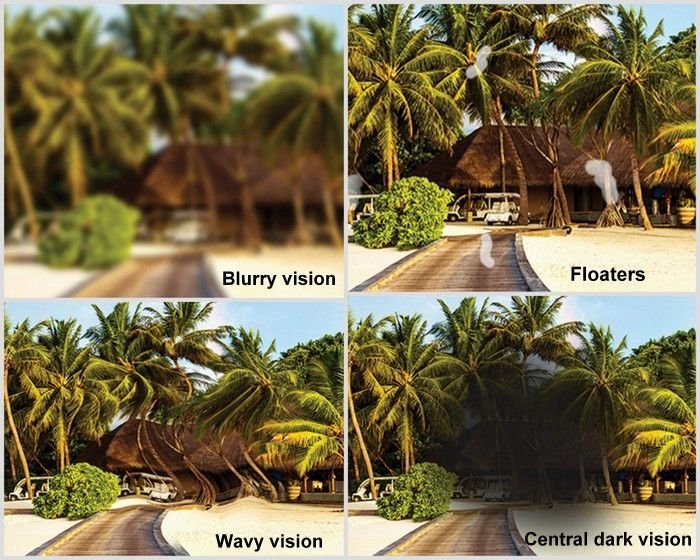
• Gradual vision loss.
• Sudden loss of vision
• Blurred vision.
• Eye pain or redness of the eye.
• Spots or dark strings floating in your vision (floaters).
• Fluctuating vision
• Dark or empty areas in your vision.
CAUSES :
Over time, too much sugar in your blood can lead to the blockage of the tiny blood vessels that nourish the retina, cutting off its blood supply. As a result, the eye attempts to grow new blood vessels. But these new blood vessels don't develop properly and can leak easily.
Types Of Diabetic Retinopathy:
Early diabetic retinopathy:
In this more common form — called nonproliferative diabetic retinopathy (NPDR) — new blood vessels aren't growing (proliferating).
Advanced diabetic retinopathy:

Diabetic retinopathy can progress to this more severe type, known as proliferative diabetic retinopathy. In this type, damaged blood vessels close off, causing the growth of new, abnormal blood vessels in the retina. These new blood vessels are fragile and can leak into the clear, jellylike substance that fills the center of your eye (vitreous).
Eventually, scar tissue from the growth of new blood vessels can cause the retina to detach from the back of your eye. If the new blood vessels interfere with the normal flow of fluid out of the eye, pressure can build in the eyeball. This buildup can damage the nerve that carries images from your eye to your brain (optic nerve), resulting in glaucoma.
When to see an eye doctor:
Careful management of your diabetes is the best way to prevent vision loss. If you have diabetes, see your eye doctor for a yearly eye exam with dilation — even if your vision seems fine.
Developing diabetes when pregnant (gestational diabetes) or having diabetes before becoming pregnant can increase your risk of diabetic retinopathy. If you're pregnant, your eye doctor might recommend additional eye exams throughout your pregnancy.
Contact your eye doctor right away if your vision changes suddenly or becomes blurry, spotty or hazy.
Risk factors:



• Patients with high blood sugar.
• People with high blood pressure.
• Those with fat.
• Pregnant women.
• Having diabetes for a long time
• Poor control of your blood sugar level
• High cholesterol
• Tobacco use
• Being Black, Hispanic or Native American.
DIAGNOSIS
1.Retinal Examination:
The damage can be detected by looking at or filming the retina.
INSTRUMENTS USED:
Ophthalmoscope:
Direct Indirect


This instrument helps the doctor to visualize the retina.
2. Optical Coherence tomography (OCT):
Images with this test will show swelling of the retina. Provide cross-sectional images of the retina. This will help determine how much fluid has leaked into the retinal tissue. OCT exams can then be used to monitor how the treatment is working.


Optical Coherence tomography (OCT) PICTURES BEING TAKEN AT - Dr. SURESH EYE HOSPITAL.
3. FUNDUS CAMERA
The state-of-the-art Cannon camera captures nerves accurately.

FUNDUS CAMERA AND FUNDUS PICTURES BEING TAKEN AT - Dr. SURESH EYE HOSPITAL
4. ultrasonography (B-Scan)
Eye B-scan ultrasonography can be very effective in patients with hemorrhage (viterous hemorrhage) or cataract. There the retina cannot be seen directly on eye examination. B-scan (ultrasonography) can detect retinal nerve abnormalities and other retinal diseases such as hemorrhage , vitreous dislocation (PVD) or retinal detachment.


B-Scan PICTURES BEING TAKEN AT - Dr. SURESH EYE HOSPITAL
TREATMENT:
1. MEDICATION:


Non steroidal anti inflammatory drugs like Nepefenac or Bromefenac are commonly used with tear substitudes.
2. Laser treatment
During laser treatment, high-intensity light rays are injected and clog the capillaries that cause bleeding. Closing the blood vessels may not be able to restore your lost vision. But there will be no further bleeding from the capillaries. Thus preventing the retinal condition from getting worse. Drops are applied to relieve pain in the eyes.
Drops are applied to the cornea to dilate the eyes. The light rays used by the contact lens are focused on the retina. The whole procedure takes 20-40 minutes. So there will be no need to stay in the hospital.


LASER TREATMENT IS BEING CARRIED OUT AT - Dr. SURESH EYE HOSPITAL.
Laser treatment
Side effects: -

• Blurred vision
• Blinking when looking at light.
• Feeling of pain or discomfort.
After effects: -

• Decreased vision at night.
• Lateral view will be partial .
• Bleeding in the eyes.
• Feeling like an insect flying while watching
Focal method: - One session treatment for a specific area.Pan Retinal method: - A partial treatment before several sessions. Treatment covers all treatable retinal areas
3. Anti-VEGF injection

Anti Endothelial growth factor (Anti-VEGF) injections are injected into the eye according to the level of the inflammation. They help prevent the growth of new blood vessels and reduce fluid accumulation. They contain many drugs such as Avastin, Razumab Lucentis and Accentrix .
When drugs called endothelial growth factor inhibitor (ANTI-VEGF) are injected into the eye, the growth of new blood vessels is prevented. New blood vessels are dangerous because they grow abnormally. These veins cause bleeding into the eyes. Some patients may be prescribed steroids if the ANTI-VEGF medication does not work. These injections are carefully given into the eyes with a very thin needle. Some people may need a retinal injection every month. It will be decided by the retinal specialist depending on the severity of the disease during re-examination.


(ANTI-VEGF) INJECTION IS BEING GIVEN AT - Dr. SURESH EYE HOSPITAL
Side effects

• Eye irritation.
• Bleeding.
• Feeling like an insect flying in the eye when looking
• Increased pressure in the eyes
• Infection
• Very few people with heart disease or high blood pressure are at risk for blood vessel damage.
Nerve hemorrhage
Bleeding and fluid leakage can occur from weakened blood vessels. Vision may be affected by bleeding.
4. Surgery:
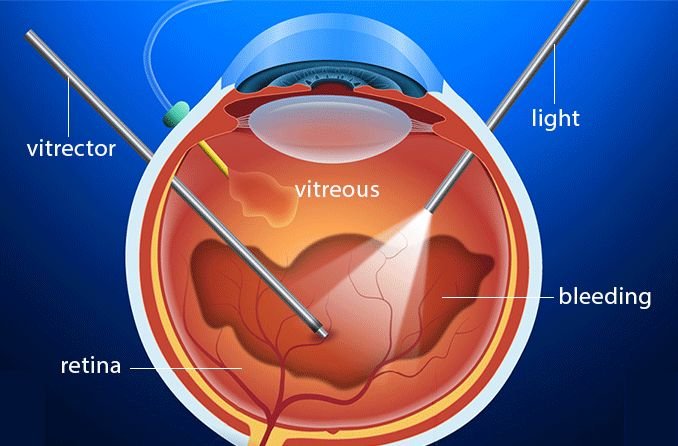
Vitrectomy surgery: -
Vitrectomy surgery is performed to cure diabetic retinopathy. At the back of the eye is a jelly-like fluid called vitreous. Vitrectomy is a surgery used to remove or replace this fluid. Retinal detachment surgery takes want to 1-2 hours .
• This is a major surgical procedure anesthetized with injection given near the eyes.
• Vitreous will be removed.
• The posterior chamber is filled with gas or silicon oil.
.jpg)


VITRECTOMY SURGERY IS BEING DONE AT - Dr. SURESH EYE HOSPITAL
After surgery, the oil will be removed within 3 - 6 months if your eye jelly (Vitreous) is replaced with silicon oil.
Before surgery: -
• A thorough physical examination should be performed
• No need to stay in the hospital. Return home in the evening.
After surgery: -
• Use drops as directed by your doctor.
• Do not do hard work.
• Must lie in a cot for 15 days
Complications:
Diabetic retinopathy involves the growth of abnormal blood vessels in the retina. Complications can lead to serious vision problems.
Vitreous hemorrhage:

The new blood vessels may bleed into the clear, jelly like substance that fills the centre of your eye. If the amount of bleeding is small, you might see only a few dark spots (floaters). In more-severe cases, blood can fill the vitreous cavity and completely block your vision.
Vitreous hemorrhage by itself usually doesn't cause permanent vision loss. The blood often clears from the eye within a few weeks or months. Unless your retina is damaged, your vision will likely return to its previous clarity.
Retinal detachment:
The abnormal blood vessels associated with diabetic retinopathy stimulate the growth of scar tissue, which can pull the retina away from the back of the eye. This can cause spots floating in your vision, flashes of light or severe vision loss.
Glaucoma:
New blood vessels can grow in the front part of your eye (iris) and interfere with the normal flow of fluid out of the eye, causing pressure in the eye to build. This pressure can damage the nerve that carries images from your eye to your brain (optic nerve).
Blindness:

Diabetic retinopathy, macular edema, glaucoma or a combination of these conditions can lead to complete vision loss, especially if the conditions are poorly managed.
Prevention
You can't always prevent diabetic retinopathy. However, regular eye exams, good control of your blood sugar and blood pressure, and early intervention for vision problems can help prevent severe vision loss.
If you have diabetes, reduce your risk of getting diabetic retinopathy by doing the following:
Manage your diabetes.


Make healthy eating and physical activity part of your daily routine. Try to get at least 180 minutes (3 hours) of moderate aerobic activity, such as walking, each week. Take oral diabetes medications or insulin as directed.
Monitor your blood sugar level.

You might need to check and record your blood sugar level several times a day — or more frequently if you're ill or under stress. Ask your doctor how often you need to test your blood sugar.
Ask your doctor about a glycosylated hemoglobin test:
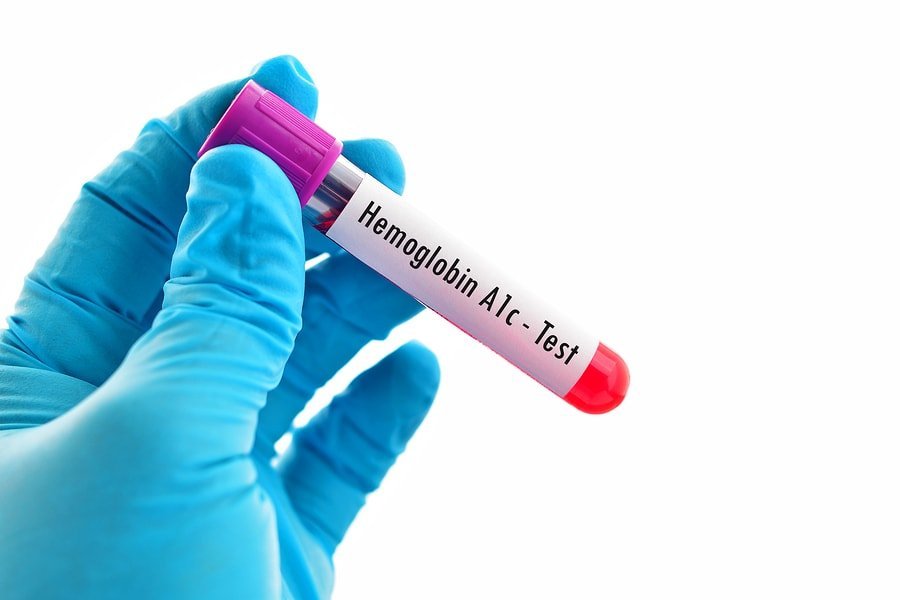
The glycosylated hemoglobin test, or hemoglobin A1C test, reflects your average blood sugar level for the two- to three-month period before the test. For most people with diabetes, the A1C goal is to be under 7%.
Keep your blood pressure and cholesterol under control.


Eating healthy foods, exercising regularly and losing excess weight can help. Sometimes medication is needed, too.
If you smoke or use other types of tobacco, ask your doctor to help you quit.

Smoking increases your risk of various diabetes complications, including diabetic retinopathy.
Pay attention to vision changes.
Contact your eye doctor right away if your vision suddenly changes or becomes blurry, spotty or hazy.
Frequently asked questions:
1. Which doctor should be consulted for Diabetic Retinopathy?
Your general practitioner should refer you to an ophthalmologist or an eye doctor.
2. How can I protect my eyes from the effects of Diabetes?
• Keep your blood sugar under control by adjusting your diet and taking medications as advised by your doctor
• Keep your blood pressure and cholesterol under control
• Exercise regularly
• Get a regular check up with an Ophthalmologist, at least once a year
3. Can Diabetes make me blind?
Diabetic retinopathy, if untreated can lead to blindness. However, if detected on time, damage to the retina can be controlled with proper treatment.
4. How long does it take for Diabetic Retinopathy to develop?
In patients of Type I DM, screening for Diabetic Retinopathy is generally started after 5 years of diagnosis. However, in patients of Type II DM, screening is started immediately on diagnosis.
5. Is diabetic retinopathy a common disorder?
In The estimates in 2019 showed that 77 million individuals had diabetes in India, which is expected to rise to over 134 million by 2045. Approximately 57% of these individuals remain undiagnosed. Diabetic retinopathy is one of the leading causes of blindness in industrialized countries.
6. What are the symptoms of diabetic retinopathy?
Diabetic retinopathy is a painless disease. Perceptible symptoms (the main one is vision loss) may not appear until late in the progression of the disease, when complications.
7. What causes diabetic retinopathy?
Diabetic retinopathy, as its name indicates, is caused by diabetes. Hyperglycemia (high blood sugar) can cause the walls of the tiny blood vessels in the retina (retinal capillaries) to gradually become fragile, swell and leak fluid (plasma) and blood.
8. Does diabetic retinopathy always progress at the same pace?
The progression of diabetic retinopathy varies. It can, however, progress more quickly in case of poor blood sugar control, high blood pressure, pregnancy, puberty or cataract surgery.
9. What are the forms of diabetic retinopathy?
There are two forms of diabetic retinopathy: nonproliferative diabetic retinopathy and proliferative diabetic retinopathy. In nonproliferative diabetic retinopathy, the blood vessels, which have become fragile due to an excess of blood sugar, start to leak fluid (plasma) and blood, and this can cause the retina to swell. In proliferative diabetic retinopathy (an aggravation of nonproliferative diabetic retinopathy) small abnormal blood vessels form, invading the retina. These blood vessels can break, causing hemorrhages.
10. What is macular edema?
Macular edema is a complication of nonproliferative as well as proliferative diabetic retinopathy (and of other diseases, particularly vein occlusions). It is a swelling of the macula (the central area of the retina) caused by leakage of fluid and blood through the walls of dilated blood vessels. Macular edema is the most common cause of vision loss.
11. How do you know if you have Diabetic Retinopathy?
As diabetic retinopathy is a disease that remains asymptomatic until a very advanced stage, the importance of regular eye examinations cannot be overemphasized, especially for people who are diabetic. An optometrist or ophthalmologist can detect DR by examining the back of the eye (ocular fundus examination), which will also indicate the type and severity of the disease.
12. Does diabetic retinopathy cause blindness?
Yes, but only in very rare cases. Diabetic retinopathy can cause blindness at a very advanced stage if necessary measures (screening, preventionand treatment) have not been taken in time.
13. Can vision loss as a result of diabetic retinopathy be prevented?
Yes. Vision loss can usually be prevented in people with diabetes by regular eye examinations throughout their lifetime. In addition, the better the diabetes control, the better the chances of preventing complications that could lead to vision impairment.
14. When is an emergency visit required?
An emergency consultation with a vision specialist is required when a sudden major change in vision is noticed.
15. Can diabetic retinopathy be triggered by certain drugs?
To date, no drugs have been associated with the onset of diabetic retinopathy. However, certain drugs promote dilation of blood vessels and can accelerate the progression of diabetic retinopathy. Doctors know whichdrugs to avoid and, when necessary, will recommend moreappropriate treatments.
16. Can diabetic retinopathy be prevented?
Diabetic retinopathy is a disease that can be prevented,mainly through the management of diabetes.
17. Can diabetic retinopathy be cured?
There is no treatment for the nonproliferative form of diabetic retinopathy withoutmacular edema, but its progression can sometimes be slowed by regular eye examinations and satisfactory management of diabetes and other aggravating disorders, such as high blood pressure. The proliferative form can be stopped. Available treatments can often lead to an improvement in vision.
18. Can the progression of diabetic retinopathy be slowed?
Yes. Existing therapies have proven effective in slowing the progression of symptoms of diabetic retinopathy. Even better, certain treatments can actually improve vision.
19. Can an operation be performed?
A vitrectomy, a surgical operation in which the vitreous humour is removed from the eye, can be performed in case of massive or chronic vitreal hemorrhage, retinal detachment and some cases of macular edema.
20. If one eye is affected, will the other be automatically affected?
The signs and symptoms of diabetic retinopathy can appear in one eye only, but usually both eyes are affected—though not necessarily equally.
21. How often should a specialist be consulted?
Monitoring by an optometrist or an ophthalmologist is indispensable if you have diabetic retinopathy. The treatment required and the frequency of visits will be determined by your vision specialist.
22. Is diabetic retinopathy painful?
No, diabetic retinopathy is not painful. The eye examinations required and the treatments available are not painful either.
23. Can you drive if you have diabetic retinopathy?
Most people with diabetic retinopathy keep their driver’s licence. Corrected visual acuity must be at least 6/12 to drive in India.
24. Can you get around on your own if you have diabetic retinopathy?
Yes. In the vast majority of cases, people with diabetic retinopathy can get around on their own. Certain tools have been developed to make it easier for people with a vision impairment associated with advanced diabetic retinopathy to get around.
25. Are there vision aids that can help?
There are numerous vision aids (magnifiers, closed circuit televisions, etc.) that facilitate daily activities for people with advanced Diabetic Retinopathy.
26. Is it possible to recover vision lost as a result of diabetic retinopathy?
Yes. Vision often improves with treatment (laser photocoagulation, antiangiogenic drugs or vitrectomy). However, diabetic retinopathy sometimes results in permanent vision loss.
27. Should people with diabetic retinopathy change their diet?
A very well-balanced diet and certain food guidelines are recommended for people with diabetic retinopathy. Sugars and fats, which increase blood sugar levels, must be avoided.
28. Should people with diabetic retinopathy quit smoking?
It’s always a good idea to quit smoking. Smokers are at greater risk of cardiovascular disease, high blood pressure in particular—a risk factor in diabetic retinopathy.
29. Will new treatments be able to cure diabetic retinopathy?
New treatments available in the last few years have considerably improved the life of people with diabetic retinopathy by slowing the progression of the disease and reducing symptoms. Research is on-going, giving hope that future therapies will be even more effective in minimizing complications and perhaps even, one day, preventing the disease—or at least delaying its onset.

{{r.reply}}
Your comment was submitted for review. It will start display once it was approved by Admin
Comments