.jpg)
Tests for Diagnosing Migraine Headaches
PLEASE CLICK HERE FOR MORE DETAILS ABOUT: MIGRAINE
1. Slit Lamp Examination:

A slit lamp is a microscope with a bright light used during an eye exam. It gives your ophthalmologist a closer look at the different structures at the front of the eye and inside the eye. It’s a key tool in determining the health of your eyes and detecting eye disease.This is done to detect any external changes in the eye.
2. Non Contact Tonometer:

An eye pressure test performed by an eye doctor will rule out glaucoma or pressure on the optic nerve as a cause of headaches.
3. Fundus Camera:

1.jpg)
The state-of-the-art Cannon camera captures nerves accurately.
You might need to take more tests to look for other medical conditions that may be causing your headaches or migraines. Keep in mind that most of these laboratory tests are not helpful in diagnosing migraine, cluster, or tension headaches.
Blood chemistry
These tests may determine many medical conditions, including diabetes, thyroid problems, and infections, which can cause headaches.
Neuroimaging in migraine:
There is no necessity to do neuroimaging in patients with headaches consistent with migraine who have a normal neurologic examination, and there are no atypical features or alarm signs present.
Criteria for ordering an MRI:
Neuroimaging may be performed for presumed migraine for the following reasons: unusual, prolonged, or persistent aura; increasing frequency, severity, or change in clinical features, first or worst migraine, migraine with brainstem aura, migraine with confusion, migraine with motor manifestations (hemiplegic migraine), late-life migraine accompaniments, aura without headache, side-locked headache, and posttraumatic headache.
CT scan.

This is a test in which X-rays and computers are used to produce an image of a cross-section of the body. A CT scan of the head may be recommended to rule out other conditions if you are getting daily or almost daily headaches.
MRI.

This test produces very clear pictures, or images, of the brain without the use of X-rays. It uses a large magnet, radio waves, and a computer to produce these images. An MRI may be recommended if you are getting daily or almost daily headaches. It may also be recommended if a CT scan does not show definitive results. In addition, an MRI scan is used to evaluate certain parts of the brain that are not as easily viewed with CT scans, such as the spine at the level of the neck and the back portion of the brain.
Sinus X-ray.
Although the CT scan and MRI provide more details, your doctor may use this test if your symptoms seem to indicate sinus problems.
EEG.
Electroencephalogram is not a standard part of a headache evaluation, but may be performed if your doctor suspects you are having seizures.
Spinal tap.
This is the removal of fluid from your spine. It looks for conditions such as infections of the brain or spinal cord.
TREATMENT OF MIGRAINE:
It should be explained to the patient that migraine is a recurrent and episodic disease that currently has no cure and that in general allows an adequate quality of life when it is known and treated. Inadequate treatment of migraine attack has a huge socio-economic impact and also increases the risk of transformation of migraine into its chronic forms.
Migraine treatment consist of non-pharmacologic and pharmacologic options.
Non-pharmacologic:
Lifestyle modifications:
Lifestyle factors of sleep, meal habits, stress and physical exercise routine are known to be related to migraine evolution. An observational study of 350 migraine patients showed that chronic migraine individuals exhibit significantly less regular lifestyle behaviors of sleep, exercise and meal time that episodic migraine patients. Perceived stress scores are higher in chronic migraine patients compared to controls. The relationship between headache and sleep is bidirectional: suboptimal sleep habits can worsen migraine frequency and migraine can decrease the quality of sleep.


The five factors identified as the most common triggers of migraine are: stress, fasting, atmospheric changes, sleep-related factors, and in women hormonal fluctuations.12 Triggers should be addressed in the anamnesis and recommendation of lifestyle changes should be made for all patients.
Performing a headache calendar should be the first step in every patient with migraine, allowing the physician to monitor the interventions in a quantitative way (i.e., changes in the total number of headache days per month). Even though, the global status of the patient should be taken into consideration, as some patient may experience very few headache days and still be incapacitated.
Attending to the evidence provided in the referred studies, the 6 most important aspects in the migraine non-pharmacological treatment are:

1. Set routines.
2. Abundant hydration.
3. Aerobic exercise.
4. Avoiding fasting.
5.Relaxation therapies
Other important aspects are:

• Excess or abstinence in regular caffeine drinkers can make migraines worse. Migraine patients should be recommended not to exceed 200mg/day and, keep their caffeine drinking as consistent as possible to avoid withdrawal headache.

• Evaluate aspartame intake, as it has been described as a strong trigger for migraine and should be avoided.
• Temporo-mandibular joint (TMJ) review, if there is any clenching activity with TMJ dysfunction a dental splint might be helpful such as the nociceptive trigeminal inhibition tension suppression system (NTI-TSS) splint. Clenching frequently occurs in migraine patients and can often cause a sensation of ear fullness. TMJ disorders have been associated with migraine chronification.
• Several studies have tried to demonstrate the effectiveness of some alternative treatment. Among them it is worth mentioning magnesium (400–600mg/day) and riboflavin (400mg/day).

• Proper head posture: Any activity, which promotes a head forward posture, will worsen symptoms, such as slumping forward at a low workstation.
• Physical therapy is an important modality in the management of headache symptoms, such as termed scapular stabilization and neck manipulations.
Pharmacologic:
Acute migraine treatment:

One of the most important aspects is to teach the patient to identify their migraine attacks because early treatment is essential to get an adequate response to end the attack. A stratified treatment must be carried out from the beginning, choosing the drug according to the severity of the symptoms, route of administration characteristics and comorbidity of the patient.
Migraine acute therapy can be divided into specific, non-specific and adjuvant treatments.
Non-specific acute treatment:
There is good quality evidence supporting the use of acetaminophen, nonsteroidal antinflammatory drugs (NSAIDs), such as acetylsalicylic acid (ASA), ibuprofen, diclofenac, and dexketoprofen. These therapies can control mild migraine attacks and auras on their own. In the specific case of paracetamol (acetaminophen) is less potent and it may be a useful first choice drug for acute migraine in those with restriction to, or who cannot tolerate, NSAIDs or aspirin. It is generally only recommended in gestational migraine, during adolescence-childhood and in attacks without a severe level of disability.
Adjuvant medications are primarily antiemetic/neuroleptics Dopamine D2 receptor antagonists, (domperidone, metoclopramide, Chlorpromazine), that are necessary in patients with nausea or vomiting which also supports the absorption of the rest of the treatment. When using these treatments, you should monitor the potential extrapyramidal side effects and concern over potentially permanent tardive dyskinesia, sedation and orthostatic hypotension.
It is strongly recommended to avoid morphs and combinations of analgesics with barbiturates, codeine, tramadol and/or caffeine, because it is associated with headache chronification and development of medication overuse headache.
Specific acute treatment:

They are the drug of choice for a moderate-severe attack and every migraine patient should be prescribed a triptan. Triptans are specific migraine drugs with proven efficacy and safety in several clinical trials, however due to its vasoconstriction effect they are contraindicated in patients with uncontrolled hypertension, coronary, cerebrovascular and peripheral vascular disease. The most frequent side effects are palpitations, neck or chest tightness, dysgeusia, laryngeal discomfort and should always be warned to the patient when prescribed. Despite these effects, it should be pointed out that they are extraordinarily safe at the vascular level.
There are 7 triptans currently available and the choice of one or the other must be individualized based on time of migraine onset (night or day), severity onset (rapidly or progressive), presence and timing of nausea or vomiting, levels of disability and frequency and pattern of attacks.
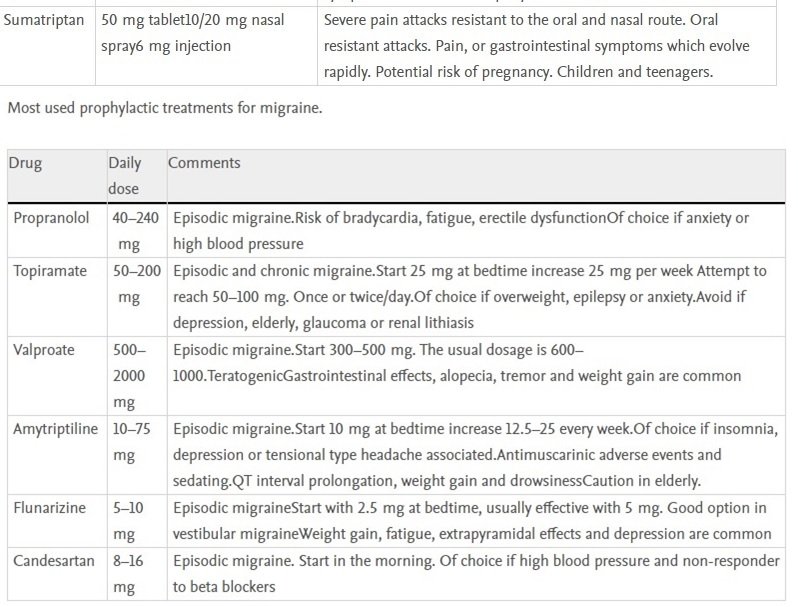
Blood pressure medications:
Beta/blockers are one of the most commonly used class of drugs in the preventive treatment of episodic migraine and are about 50% effective in producing a greater than 50% reduction in attack frequency. Of these, propranolol is the most evidence-based and widely used drug although it has the disadvantage of not being taken once daily like the other beta-blockers. Although the available evidence is limited, lisinopril and overall candesartan are effective for episodic migraine prevention and may be an option in those migraineurs who associate high blood pressure but have contraindicated the use of beta-blockers.27 According to the available evidence, from this pharmacological group, flunarizine, a non-specific calcium channel blocker, is the only effective treatment in the prophylaxis of episodic migraine.
.jpg)
2.jpg)
{{r.reply}}
Your comment was submitted for review. It will start display once it was approved by Admin
Comments