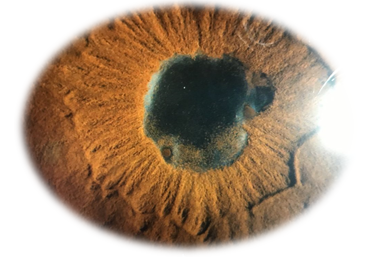
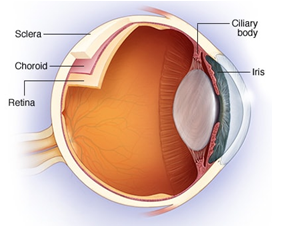
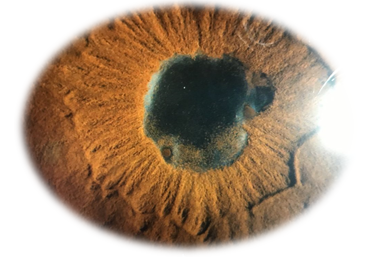
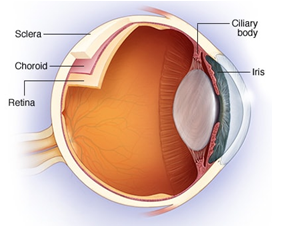
Uveitis is a general term describing inflammation of the part of the eye called the uveal tract. This consists of the iris, ciliary body and choroid - although uveitis can additionally involve other parts of the eye. It can be caused by diseases or problems of the eye alone, or can be a part of conditions affecting other parts of the body.
Uveitis is inflammation of the uveal tract. The uveal tract is the name given to the part of your eye that is made up of:
• The iris: the part of your eye that gives it colour.
• The ciliary body: a small ring-like muscle that sits behind your iris and which helps the eye to focus.
• The choroid: the layer of tissue between your retina and your sclera, containing blood vessels and a pigment that absorbs ex-cess light.
The uvea contains most of the eye's blood vessels.
(PLEASE CLICK HERE FOR TAMIL IMAGE FORMAT: UVEITIS)


How common is uveitis and who develops it?
It is thought that between 10 and 50 per 100,000 people develop uveitis each year in the India. It mostly affects people between the ages of 20 and 59 and is uncommon in children. However, uveitis can affect anyone of any age. If you have one of the underlying conditions or problems mentioned above, you are at greater risk of developing uveitis. In countries of the developed world, such as the India, uveitis is the cause of visual impairment in about 1 in 10 people.
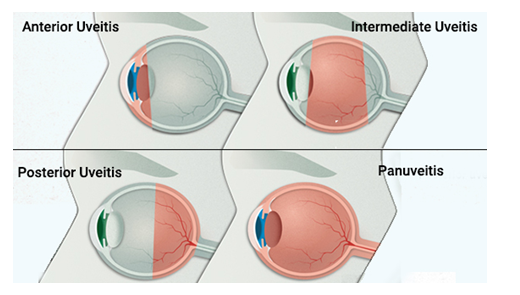
What are the different types of uveitis?
Uveitis is classified according to the part of the uveal tract that the inflammation affects:
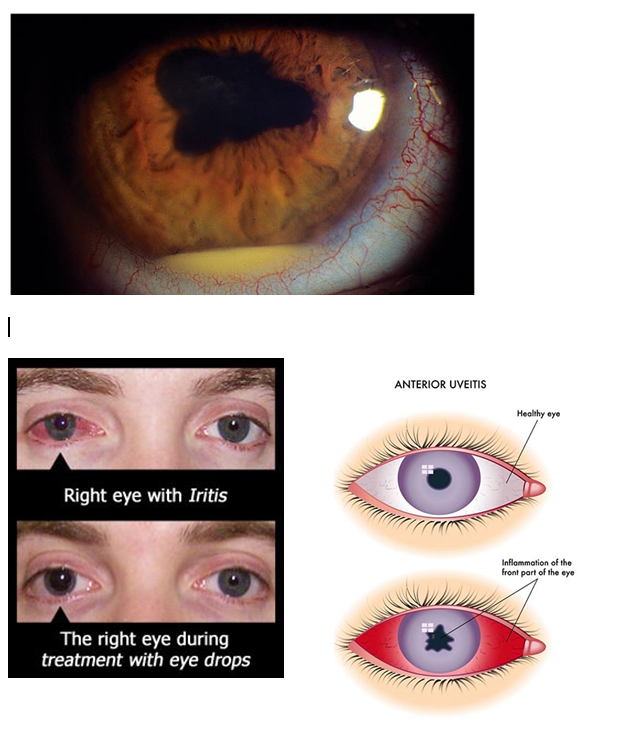
• Anterior uveitis
Anterior uveitis is the term for inflammation which affects the eye's front (anterior) part of the uveal tract. This can include the iris (iritis) or the iris and the ciliary body (iridocyclitis). It is the most common type of uveitis and the most painful. It is most often caused by inflammatory diseases, infections or trauma.
• Intermediate uveitis
Intermediate uveitis is the term for inflammation which affects the middle part of the uveal tract or eye, mainly the vitreous humour. It can also affect the underlying retina. It has been linked to several dis-eases,including sarcoidosis.
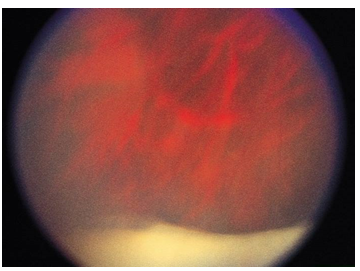
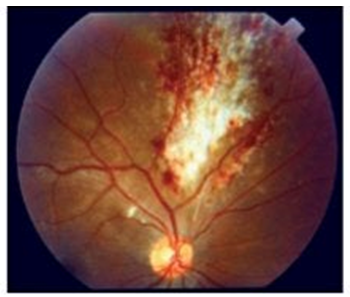
Posterior uveitis is the term for inflammation which affects the back (posterior) part of the eye. It can affect the choroid, the head of the optic nerve, and the retina (or any combination of these structures). It includes chorioretinitis, retinitis and neuroretinitis. Posterior uveitis is the least com-mon form of uveitis.
Panuveitis uveitis:
• Panuveitis is the term for inflammation affecting the whole of the uveal tract. This is the most serious form. Behçet's disease is one of the most com-mon causes and it can severely damage the retina.
Intermediate, posterior and panuveitis are the most likely forms of uveitis to affect vision, and the most recurrent forms.
Uveitis can be:
• Acute: the uveitis is of sudden onset and lasts less than three months (attacks in this form usually last around six weeks).
• Chronic: this means it is persistent. The uveitis lasts for more than three months.
• Recurrent: the disease can flare up (relapse) and, at other times, it settles down. Recurrence is very common, although the time between attacks is very variable.
The reason why some people develop chronic uveitis is not known. It is not thought to be due to inadequate treatment.
What causes Uveitis?
Idiopathic:
Majority of the uveitis causes occur with no known reason. It is also thought that 'idiopathic' uveitis may, in fact, have an autoimmune basis.
Autoimmune and inflammatory diseases:
Our immune system normally makes small proteins (antibodies) to attack bacteria, viruses and other 'germs'. In people with autoimmune diseases, the immune system makes antibodies against the tissues of their body, causing damage and inflammation. It is not clear why this happens.
• Autoimmune diseases that are associated with uveitis include rheumatoid ar-thritis and Behçet's disease” . People with some other inflammatory diseases are also more prone to uveitis. Such diseases include
• ankylosing spondylitis
• reactive arthritis
• sarcoidosis
• psoriasis
• inflammatory bowel disease (including Crohn's disease and ulcerative colitis).
Infection:
Various types of infections caused by germs (bacterial, fungal and viral) can cause inflammation of your eye and uveitis. Infections include
• toxoplasmosis (the most common infectious cause of anterior uveitis)
• herpes simplex
• herpes zoster
• cytomegalovirus
• gonorrhoea
• tuberculosis
• Lyme disease
• HIV
• syphilis are rare infectious causes
Injury to the eye
Uveitis can occur after injury to your eye.
Iatrogenic causes
'Iatrogenic' refers either to an unforeseen or to an inevitable side-effect from a medical treatment. In this case, iatrogenic uveitis is usually uveitis that has resulted from eye surgery. Rarely, uveitis can occur as a side-effect of some medicines. Examples include rifampicin (used to treat tuber-culosis) and cidofovir (used to treat human cytomegalovirus infec-tion).Cidofovir is used as Aids to treat infections.
Cancers:
Some cancers are associated with inflammation and uveitis. These in-clude leukaemia, lymphoma and ocular malignant melanoma but all are rare causes of uveitis.

Some cancers are associated with inflammation and uveitis. These include leukaemia, lymphoma and ocular malignant melanoma - but all are rare causes of uveitis.
How is uveitis diagnosed?
Uveitis is usually suspected on the basis of the symptoms that you have. If your doctor suspects that you have uveitis, you will usually be referred to an eye specialist for further examination and confirmation. The doctor may start by testing your vision. This allows them to assess any differences in vision between your eyes. It also means that they can tell if the uveitis is causing your vision to worsen.
The doctor examining your eye will use a special microscope called a slit-lamp to examine your eye. If you have uveitis, the doctor will see some specific signs of inflammation in your eye that will allow them to make the diagnosis.
You may need further investigations, especially if the doctor thinks there may be an underlying problem. You may also need further investigations if you have had previous episodes of uveitis, or if this episode is severe or affects both eyes. These tests may include optical coherence tomography (OCT), which takes special pictures of your eye, blood tests and possibly also a chest X-ray.

NON CONTACT TONOMETER:
A non-contact tonometer uses a small puff of air (which is why it's many times referred to as the "puff test") to measure an eye's pressure.
FUNDUS CAMERA:
A fundus camera or retinal camera is a specialized low power microscope with an at-tached camera designed to photograph the interior surface of the eye, including the retina, retinal vasculature, optic disc, macula, and posterior pole.
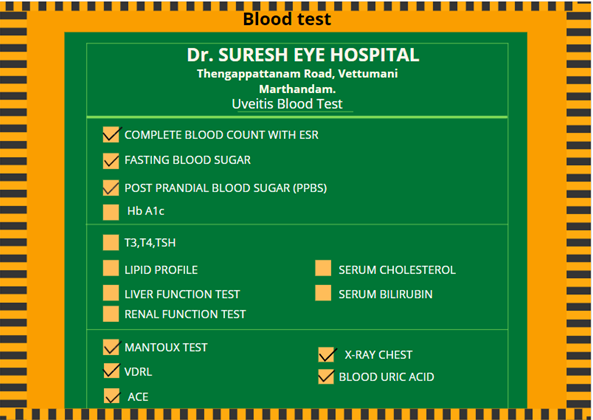
LIST OF COMMON BLOOD TESTS CARRIED OUT FOR UVEITIS:
What is the treatment for uveitis?
Treatment for uveitis aims to help relieve pain and discomfort in the eye(s), treat any underlying cause (if possible) and reduce the inflammation. This may prevent permanent loss of vision or other complications. Treatment usually includes the following:
Steroid eye drops:
• Steroid eye drops are usually used to reduce the inflammation in uveitis. Steroid drops are the main treatment for uveitis and may be the only treatment for mild attacks. Examples of steroid drops in clude prednisolone and dexamethasone eye drops.
• Although steroid eye drops usually work well, in some cases side-effects occur and these are sometimes serious. Therefore, steroid eye drops are usually only prescribed by an eye special-ist (an ophthalmologist) who can monitor the situation. It is particularly important to be certain that you don't have herpes simplex virus (also called cold sore virus) infection of your eye before steroids are used.
• Possible side-effects that sometimes occur include ulcers on the cornea of the eye, which can be very painful and affect your vision. If steroid eye drops are used for long periods of time, they can lead to clouding of your lenses (cataracts) or to raised pressure in your eye (glaucoma).
Treatment to relieve pain and discomfort:
Cycloplegic eye drops: these are eye drops that relieve pain by causing the pupil in your eye to widen (dilate) by relaxing the muscle in the ciliary body. As a result, the inflamed iris is able to rest and recover. Examples in-clude atropine and cyclopentolate eye drops. There are some side-effects. They can make your pupil appear large, and can cause temporary blurred vision and difficulty with focusing. When the effect of the drops wears off, these side-effects disappear. If these drops are not used, the inflammation in the iris may cause it to become 'stuck' to the lens, causing permanent scarring.
Dark glasses: if your symptoms include sensitivity to bright light (photophobia), wearing dark glasses may be helpful.
• Painkillers: 
painkilling medication, such as paracetamol, may also help.
Steroids by mouth or injection:
In severe uveitis, steroids are sometimes given by injection into or around your eye. They can also be given by mouth. These can have side-effects if used in the long term. The main side-effects from oral steroids occur when they are used for more than a few weeks. These include 'thinning' of the bones (osteoporosis), thinning of the skin, weight gain, muscle wasting and a generally increased risk of infection.
Immunosuppressive medicines:
If steroid treatment is needed in the longer term to treat uveitis, a second medi-cine known as an immunosuppressive medicine may be used. This can help to reduce the amount of steroids needed and/or help to control the uveitis if ster-oids are not working.
Biological agents:
There are a number of new treatments for uveitis that are currently being inves-tigated. These include medicines called TNF alpha-blockers, such as etanercept and infliximab.
Treatment of underlying conditions and causes:
If there is an underlying cause of your uveitis this also needs to be treated (if possible). This means treating any underlying infection, inflammatory disease or autoimmune disease.
Surgery:
Occasionally, surgery is needed to treat uveitis - usually persistent (chronic) uveitis. Surgery is used in addition to the other treatments mentioned above. Uveitis cannot be treated by surgery alone.
• If someone has persistent floaters that are affecting their ability to see, the vitreous humour in the eye can be removed. Floaters tend to develop because of inflammation causing damage to the vitreous humour.
• Surgery may also be used to treat cataracts or glaucoma that can occur as a consequence of steroid treatment.
What are the complications of uveitis?
If uveitis is not treated quickly, it can lead to permanent loss of vision. It may also lead to complications, such as raised pressure in your eye (glaucoma). These complications can themselves affect your eyesight. If complications are not detected early, they can sometimes have a more harmful (detrimental) effect on your eyesight than the underlying uveitis.
The complications of uveitis may be caused by the effects of the inflammation inside the eye. Some of them may also be caused by the steroid treatment used to control the inflammation. Despite this, as a general rule, using enough ster-oids to control the uveitis will generally give a better outcome than using too few steroids and not controlling the inflammation. Complications that can sometimes occur with uveitis include:
• Formation of synechiae: The name 'synechiae' is given to the 'bands' of tissue that can form between the iris and the lens due to inflammation. Eye drops which cause the pupils to widen (dilate) help to prevent synechiae.
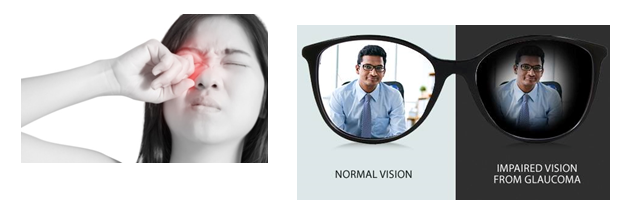
• Glaucoma:
The inflammation in your eye may cause the pressure in your eye to increase and can cause glaucoma. Using steroids can al-so cause a sudden increase in pressure in your eye, especially if you already have glaucoma. If glaucoma is not treated, it can lead to loss of vision. (PLEASE CLICK HERE FOR GLAUCOMA BLOG :GLAUCOMA)
• Macular oedema:
This is the term for fluid building up in the back of your eye around your macula on your retina. It may cause permanent visual loss. In addition, holes may form in the macula, leading to areas of lost vision on the retina.(PLEASE CLICK HERE FOR ARMD BLOG :Age Related Macular Degeneration)
• Cataract formation:
Eye inflammation can cause clouding of the lens (cataract formation). Cataracts may also be caused by long-term steroid treatment. If a cataract worsens and is not treated, it can lead to visual loss. See our blog Cataracts for more details.
• Retinal detachment:
The inflammation can cause 'pulling' on your retina so that it 'comes away' or is detached from the blood vessels below. This can cause you to experience flashing lights, floaters and problems with your vision. If you suspect that you have a retinal detachment, contact your doctor immediately, as urgent treatment is often needed. (PLEASE CLICK HERE FOR RETINAL DETACHMENT BLOG :RETINAL DETACHMENT)
What is the outlook for uveitis?
In general, the sooner treatment for front of eye (anterior) uveitis is started, the better the outlook (prognosis) and the quicker it goes away. However, anterior uveitis can come back (recur), especially if it is associated with an underlying illness such as autoimmune or inflammatory disease.
Anterior uveitis can sometimes become persistent (chronic) despite early and adequate treatment.
Intermediate uveitis and posterior uveitis are more likely to last for a longer time or to become chronically recurrent. Some people who have recurrent uveitis learn to recognise their symptoms. They are sometimes given steroid eye drops to keep in reserve and start when their usual symptoms reappear. People who have chronic or recurrent uveitis are usually under the long-term care of an eye specialist and have regular check-ups in the outpatient clinic.
Uveitis caused by infection generally clears up when the infection is treated, and does not recur.
.jpg)






.jpg)
.jpg)















.jpg)

Comments